Stem Cell-Derived Therapies for Type 1 Diabetes: A Medical Revolution or a Futile Dream?
- admin
- September 22, 2024
- 10:14 am
- No Comments

The quest to find a long-term solution for Type 1 diabetes has led researchers into the complex world of stem-cell-derived therapies.
Recently, a groundbreaking study at Harvard has shed light on the potential of using stem-cell-derived replacement therapies to regenerate insulin-producing pancreatic cells.
This approach could revolutionize diabetes treatment, reducing or even eliminating the need for insulin injections.
But is this breakthrough truly a miracle, or are we setting ourselves up for disappointment?
Article Index
- Understanding Type 1 Diabetes and the Need for Innovative Treatments
- The Promise of Stem-Cell-Derived Therapies
- Harvard’s Groundbreaking Study: Regenerating Pancreatic Cells
- Challenges and Controversies in Stem-Cell Research
- The Future of Diabetes Treatment: Miracle or Mirage?
- Conclusion: Assessing the Reality
Understanding Type 1 Diabetes and the Need for Innovative Treatments
Type 1 diabetes is an autoimmune disorder where the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas.
This leaves patients dependent on regular insulin injections to manage their blood sugar levels. Traditional treatments focus on insulin therapy and lifestyle changes, but they do not address the underlying issue of beta-cell destruction.
This is where stem-cell-derived therapies come into play, offering a potential to regenerate the lost cells.
The Promise of Stem-Cell-Derived Therapies
Stem-cell-derived therapies are on the brink of revolutionizing diabetes care.
The idea?
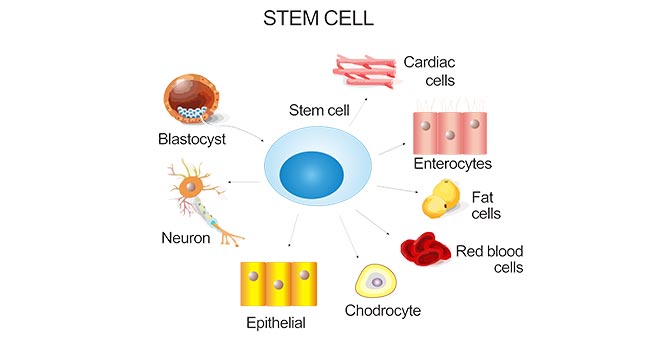
Regenerate those hard-working insulin-producing beta cells in the pancreas using pluripotent stem cells—basically the body’s master builders. These stem cells can transform into almost any cell type, including the all-important pancreatic beta cells that produce insulin.
Research from the Journal of Clinical Investigation has shown that stem-cell-derived beta-like cells (sBCs) are not just a potential long-term insulin source.
They also offer researchers a powerful window into how real human beta cells develop, respond to glucose, and dodge—or fall prey to—the immune system.
Animal studies have been especially promising. Mice and nonhuman primates receiving sBCs often achieve near-normal blood sugar levels, sometimes without needing insulin injections. Human trials are now underway.
In early-stage clinical studies—like those by Vertex Pharmaceuticals (VX-880) and ViaCyte (PEC-Direct)—some participants have shown real insulin production (as measured by C-peptide levels) and have cut back or even stopped using insulin after just a few months.
But challenges still exist. Once transplanted, these cells can face oxygen deprivation, immune rejection, and other survival issues.
To solve that, scientists are experimenting with encapsulation devices that protect sBCs while allowing nutrients to pass through, improving graft blood supply, and even using gene editing to make the cells “invisible” to the immune system.
So, while we ae not quite at the finish line, we are well past the starting block.
If ongoing clinical trials continue to succeed, a future without insulin shots could be more than just wishful thinking—it could be our next big medical reality.
Harvard’s Groundbreaking Study: Regenerating Pancreatic Cells
A recent study conducted at Harvard focused on stem-cell-derived replacement therapies for Type 1 diabetes.
The researchers developed a method to direct human pluripotent stem cells into pancreatic beta cells that can produce insulin.
This approach has shown promise in animal models, where the transplanted cells were able to restore insulin production and maintain blood glucose levels without the need for external insulin.
The study, published in the Nature Biotechnology, highlighted that the transplanted stem-cell-derived beta cells responded to glucose levels in the blood, releasing insulin when needed.
This could potentially eliminate the need for regular insulin injections, providing a more natural regulation of blood sugar levels.
Challenges and Controversies in Stem-Cell Research
Stem-cell-based therapies for Type 1 diabetes have generated enormous excitement—but along with the promise comes a cluster of scientific, medical, ethical, and logistical hurdles. Let’s unpack some of the biggest ones.
>>> First, autoimmunity remains a stubborn roadblock. Type 1 diabetes originates from the immune system attacking the body’s own insulin-producing beta cells. Even if we successfully implant stem-cell-derived beta cells, the autoimmune process may target the new cells too.
According to studies in Nature Biotechnology, researchers are now experimenting with gene editing and encapsulation techniques to “cloak” the new cells from immune detection—but these solutions are still in development.
>>> Second, differentiation inconsistency is a thorn in the side of scalability. Turning pluripotent stem cells into fully functional beta cells is far from foolproof. A paper in Stem Cell Reports found that batches of stem-cell-derived beta cells can vary significantly in insulin secretion ability, sometimes resembling fetal rather than adult cells. This variability poses a major obstacle for clinical reliability.
>>> Third, long-term viability of the transplanted cells is uncertain. For example, a 2022 study from Diabetes Research and Clinical Practice found that even when engraftment was initially successful, many beta-like cells lost functionality or died within months due to microenvironmental stress or inadequate vascularization.
>>> Add to that the high cost of manufacturing and administering stem-cell therapies, which can run into hundreds of thousands of dollars per patient. This limits access and raises concerns about healthcare equity.
>>> Finally, ethical concerns—particularly around the use of embryonic stem cells—remain controversial in many countries. Although induced pluripotent stem cells (iPSCs) offer an alternative, their genetic reprogramming poses its own safety risks, such as tumor formation.
In short, while stem-cell research offers a compelling vision for the future, the path forward is tangled in scientific unknowns, immune system battles, ethical debates, and economic constraints.
The Future of Diabetes Treatment: Miracle or Mirage?
Despite these challenges, stem-cell-derived therapies could revolutionize the way we treat Type 1 diabetes. Clinical trials are ongoing, and the initial results are promising.
For example, a study by researchers at the University of Helsinki showed that human stem-cell-derived pancreatic islets could effectively restore insulin secretion and control blood glucose levels in non-human primates.
The transplanted cells exhibited similar behavior to natural beta cells, responding to changes in blood glucose levels and secreting insulin accordingly.
Moreover, advances in gene editing and immunomodulation could help overcome the issue of immune rejection.
Techniques such as CRISPR-Cas9 are being explored to create stem cells that are invisible to the immune system, potentially reducing the risk of autoimmune attacks on the newly generated beta cells.
Conclusion: Assessing the Reality
So, is stem-cell-derived therapy for Type 1 diabetes a miracle or a mirage?
The answer lies somewhere in between. While the technology holds the potential to transform diabetes treatment by including best diabetic supplements, significant hurdles must be overcome before it can be widely adopted.
The initial results are promising, but they need to be validated through extensive clinical trials.
As research progresses, we may well see a future where insulin injections are a thing of the past, replaced by regenerative therapies that restore natural insulin production.
References: