Is LADA the Missing Link Between Autoimmunity and Diabetes Misdiagnosis?
- admin
- September 24, 2024
- 4:29 pm
- No Comments

When it comes to diabetes, the traditional distinction between Type 1 and Type 2 diabetes has been ingrained in medical thinking for years.
However, what happens when the diagnosis doesn’t fit neatly into either box?
Enter Latent Autoimmune Diabetes in Adults (LADA)—a form of diabetes that shares characteristics of both Type 1 and Type 2 diabetes, often leading to misdiagnosis and improper treatment.
Could LADA be the key to understanding the bridge between autoimmunity and diabetes misdiagnosis?
Let us dig deeper into this overlooked, yet significant, area of diabetes research.
Article Index:
- What is Latent Autoimmune Diabetes in Adults (LADA)?
- LADA: A Case of Misdiagnosis as Type 2 Diabetes
- Understanding LADA and Autoimmunity
- The Role of Autoimmune Diabetes in LADA
- Diabetes Type 1.5: Why LADA is Different
- Recognizing the Symptoms of LADA
- How is LADA Diagnosed? The Overlap with Type 2 Diabetes
- Treatment Approaches for LADA
- FAQS on LADA & Diabetes Misdiagnosis
- Conclusion: Is LADA the Missing Link?
What is Latent Autoimmune Diabetes in Adults (LADA)?
Latent Autoimmune Diabetes in Adults, often referred to as LADA, is sometimes dubbed diabetes type 1.5, as it has characteristics of both Type 1 and Type 2 diabetes.
Unlike classic type 1 diabetes, which is typically diagnosed in childhood, LADA emerges in adulthood.
However, unlike type 2 diabetes, which is related to insulin resistance, LADA is an autoimmune diabetes, meaning the body’s immune system attacks insulin-producing beta cells, much like what happens in type 1 diabetes.
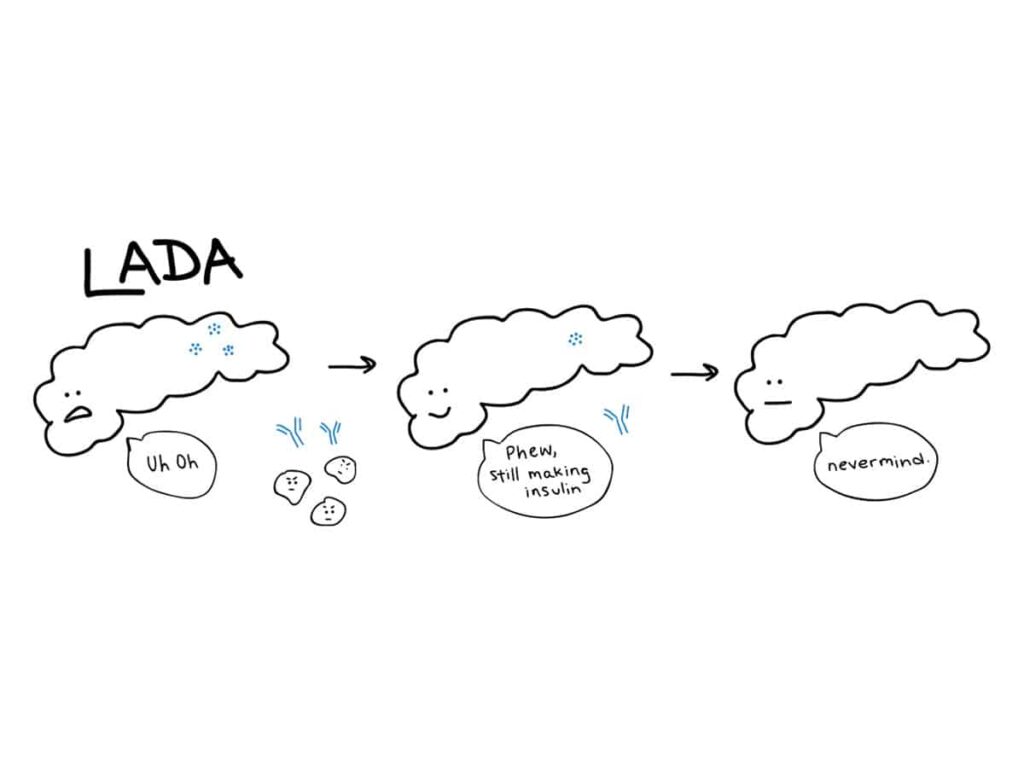
What makes LADA diabetes particularly challenging is its slower progression compared to typical Type 1 diabetes.
This slower onset often leads doctors to initially diagnose it as type 2 diabetes, resulting in patients being treated with oral medications that are more appropriate for insulin resistance.
Unfortunately, this delay in recognizing the latent autoimmune diabetes component of LADA can worsen the patient’s condition over time.
LADA: A Case of Misdiagnosis as Type 2 Diabetes
LADA is frequently mistaken for Type 2 diabetes because it tends to develop later in life—usually in people over the age of 30—and its symptoms can be initially mild.
However, unlike typical Type 2 diabetes, LADA patients eventually lose the ability to produce insulin because of the autoimmune attack on their pancreas.
Many LADA diabetes patients are initially placed on oral medications that treat insulin resistance rather than the real issue—insulin deficiency.
This misdiagnosis as latent adult diabetes (akin to Type 2) not only delays the correct treatment but also leads to confusion and frustration for both patients and healthcare providers.
Studies suggest that as many as 10% of those diagnosed with Type 2 diabetes may actually have latent autoimmune diabetes adults.
Understanding LADA and Autoimmunity
Autoimmune diseases occur when the body’s immune system mistakenly attacks its own tissues. In LADA autoimmune diabetes, the immune system specifically targets the insulin-producing beta cells in the pancreas, much like it does in Type 1 diabetes.
However, the progression in LADA DM is much slower, allowing some insulin production to persist for a few years before it declines.
Because of its autoimmune nature, LADA type 1 diabetes should be treated more like Type 1 diabetes, requiring insulin therapy as the beta cells continue to deteriorate.
However, due to the slow onset of diabetes mellitus type 1.5, there is often a period during which oral medications used for Type 2 diabetes can still seem effective, further complicating the correct diagnosis.
The Role of Autoimmune Diabetes in LADA
LADA DM sits on the spectrum of autoimmune diabetes, making it a crucial piece in the puzzle of understanding how autoimmune disorders contribute to different types of diabetes.
In autoimmune diabetes, antibodies that attack the pancreas can often be detected years before symptoms even begin.
Similarly, LADA patients often exhibit the same antibodies seen in Type 1 diabetes, such as islet cell antibodies (ICAs) and glutamic acid decarboxylase antibodies (GADAs).
A study in the Diabetes Care journal found that around 70-90% of LADA patients have GAD antibodies, providing a useful marker for diagnosis.
This autoimmune component underscores why treating LADA autoimmune diabetes with traditional Type 2 methods—focused on insulin resistance rather than insulin deficiency—can be problematic.
Diabetes Type 1.5: Why LADA is Different
The term diabetes type 1.5 LADA arose to describe this unique form of diabetes that lies between Type 1 and Type 2 diabetes.
While Type 1 diabetes involves a rapid autoimmune destruction of insulin-producing cells, and Type 2 diabetes centers around insulin resistance, diabetes mellitus type 1.5 (LADA) represents a slower autoimmune process, where beta cell destruction happens over time.
The misconception often comes from the fact that LADA shares some initial characteristics of Type 2 diabetes, such as the age of onset and mild early symptoms.
This slow progression can easily trick clinicians into treating it as Type 2.
However, because LADA involves an autoimmune response, patients ultimately require insulin therapy as their ability to produce insulin declines.
Recognizing the Symptoms of LADA
Latent autoimmune diabetes adults share many symptoms with both Type 1 and Type 2 diabetes, including increased thirst, frequent urination, fatigue, and unexplained weight loss.
However, patients with LADA diabetes are often not overweight, which is a key differentiator from many Type 2 diabetes patients.
The progression from mild to severe symptoms typically occurs over months or years.
During this time, oral medications like metformin may work for a short while, but as insulin production decreases, these medications become less effective, leading to the need for insulin injections.
How is LADA Diagnosed? The Overlap with Type 2 Diabetes
Diagnosing LADA type 1 requires a careful approach.
Standard glucose tests will show high blood sugar levels, much like with Type 2 diabetes, but the presence of autoimmune markers such as GAD antibodies will point towards LADA DM.
The problem is that many doctors do not immediately test for these antibodies unless there is a suspicion of autoimmune diabetes.
As a result, LADA type 1 often goes undiagnosed until the patient’s insulin production is so diminished that oral treatments fail to manage their blood sugar effectively.
Treatment Approaches for LADA
Since LADA autoimmune diabetes is characterized by an eventual decline in insulin production, treatment should focus on insulin therapy from the onset or as soon as insulin levels begin to decline.
Unlike Type 2 diabetes, where lifestyle changes and oral medications can often manage the disease for years, diabetes mellitus type 1.5 requires a more proactive approach in recognizing the autoimmune component and initiating insulin when necessary.
Insulin therapy helps to preserve the remaining beta cells and can delay further destruction, providing better long-term outcomes for LADA DM patients.
FAQS on LADA & Diabetes Misdiagnosis
Q-1: Why is LADA often called the bridge between Type 1 and Type 2 diabetes?
A-1: LADA (Latent Autoimmune Diabetes in Adults) shares features of both major diabetes types. Like Type 1 diabetes, it involves an autoimmune attack on insulin-producing beta cells. Like Type 2 diabetes, it develops in adulthood and often responds to non-insulin treatments at first. This overlap makes LADA easy to misclassify, even though the underlying problem is immune-driven rather than purely metabolic.
Q-2: Can LADA explain why some adults stop responding to Type 2 diabetes medications?
A-2: Yes. In LADA, beta cells are gradually destroyed by the immune system. Early on, the pancreas still produces enough insulin for medications to work. Over time, insulin production drops sharply, and drugs that improve insulin sensitivity no longer help. This sudden treatment failure often confuses both patients and doctors and leads to delayed insulin therapy.
Q-3: Is autoimmunity the main factor that separates LADA from Type 2 diabetes?
A-3: Absolutely. The presence of diabetes-related autoantibodies is the clearest difference. According to bestdietarysupplementfordiabetics.com research, “These antibodies show that the immune system is actively targeting the pancreas”. In Type 2 diabetes, insulin resistance is the main issue, not immune attack. Without antibody testing, this critical difference is often missed, leading to misdiagnosis.
Q-4: Can misdiagnosing LADA affect long-term health outcomes?
A-4: Yes. Treating LADA as Type 2 diabetes can delay proper insulin support, allowing blood sugar levels to stay high for too long. This increases the risk of complications and accelerates beta-cell loss. Early identification and tailored treatment can help preserve remaining insulin production and improve long-term control.
Q-5: Why is LADA still frequently overlooked in adults?
A-5: LADA doesn’t fit neatly into traditional diabetes categories. Symptoms develop slowly, weight may be normal, and insulin isn’t needed right away. Because routine testing focuses on glucose levels rather than immune markers, many cases remain undetected until insulin dependence becomes unavoidable. This makes LADA one of the most commonly missed forms of diabetes.
Final Call: Is LADA the Missing Link?
So, is LADA the missing link between autoimmunity and diabetes misdiagnosis?
The answer is “yes”.
Latent autoimmune diabetes exemplifies how autoimmune mechanisms can influence diabetes but in a way that often mimics Type 2 diabetes initially.
This blending of traits from both Type 1 and Type 2 diabetes is why LADA is frequently misdiagnosed, leading to improper treatment.
Recognizing LADA as a distinct form of diabetes—one that requires early and accurate detection of autoimmune markers—is key to preventing the mismanagement of patients who fall into this “grey area.”
To keep your blood sugar levels in control, opt for supplements to lower blood sugar naturally.
LADA DM holds the key to better understanding how autoimmunity can shape diabetes outcomes and pave the way for more personalized treatments that target the root causes of diabetes.
References