Are Cytokines the Hidden Culprits Fueling Type 1 Diabetes?
- admin
- October 9, 2024
- 2:24 pm
- No Comments
If you have ever dug into the mechanics of type 1 diabetes, you know it is a complex autoimmune condition.
But here is a question that does not always make the headlines: could cytokines, the small proteins secreted by immune cells, be one of the hidden culprits driving this disease?
Over the years, research has pointed to the pivotal role of cytokines in autoimmune responses, and their influence on type 1 diabetes has come under intense scrutiny.
So, let us dive deep into the science of how cytokines may be fueling type 1 diabetes—pulling from my personal journey with the disease and the research that has shaped our current understanding.
In This Article:
- What Are Cytokines and Why Do They Matter?
- How Cytokines Contribute to Autoimmune Diseases
- The Link Between Cytokines and Type 1 Diabetes
- The Role of TNF-Alpha in Diabetes
- IL-6: A Key Player in the Type 1 Diabetes Puzzle
- Cytokine Storms and Their Connection to Diabetes
- Daily Life Implications of Cytokine Activity in Diabetes
- Top 5 FAQs on Cytokines & Type 1 Diabetes
- Conclusion: Are Cytokines the Hidden Culprits?
What Are Cytokines and Why Do They Matter?
Cytokines are like the body’s messengers. They help regulate immune responses, inflammation, and cell communication.
Whether you are fighting off a cold or dealing with a more serious autoimmune condition, these proteins are on the frontline, signaling cells to fight infections or repair damage.
For someone like me with type 1 diabetes, understanding cytokines is crucial.
Why?
Because in autoimmune conditions, they can act a bit like an overzealous referee—blowing the whistle on healthy tissues, like insulin-producing beta cells in the pancreas, by marking them for destruction.
This is where things get tricky for people like me living with diabetes.
How Cytokines Contribute to Autoimmune Diseases?
Cytokines can either protect or harm the body, depending on how they are deployed.
In autoimmune diseases like type 1 diabetes, certain cytokines can turn rogue.
For instance, when I first started learning about my condition, I was surprised to discover that these little proteins were likely orchestrating the attack on my pancreas.
Cytokines can trigger immune cells to recognize beta cells as foreign invaders, leading to their destruction.
In a healthy individual, cytokines work to regulate inflammation and immune responses, but in type 1 diabetes, this regulation is out of whack.
In my case, cytokines created an inflammatory environment in my pancreas that gradually led to the destruction of the insulin-producing cells.
The Link Between Cytokines and Type 1 Diabetes
So, how does this all tie back to type 1 diabetes?
In simple terms, it is about inflammation and immune system malfunction.
The cytokines that normally protect our bodies from infection become hyperactive and direct immune cells to attack the body’s own insulin-producing beta cells.
This leads to the hallmark of type 1 diabetes: a lack of insulin production.
In my own journey with type 1 diabetes, I have come to realize how deep this immune system dysfunction goes.
What was initially a random blood sugar spike turned into a full-blown autoimmune assault on my pancreas.
Research shows that cytokines, particularly pro-inflammatory ones, play a central role in beta-cell destruction, pushing the body towards insulin dependency.
The Role of TNF-Alpha in Diabetes
TNF-alpha (tumor necrosis factor-alpha) is a well-known inflammatory cytokine, and its role in type 1 diabetes is gaining more attention.
When I first learned about TNF alpha in diabetes, I understood how chronic inflammation can lead to beta-cell destruction.
Studies show that TNF-alpha can directly damage the cells in the pancreas and impair their ability to produce insulin.
A paper in Diabetes (a leading journal in the field) explains how TNF-alpha can even trigger other immune cells to attack, exacerbating the situation.
For those of us with type 1 diabetes, this means our body is fighting a losing battle as TNF-alpha drives the process of destruction.
IL-6: A Key Player in the Type 1 Diabetes Puzzle
While TNF-alpha plays its role, interleukin-6 (IL-6) deserves its spotlight.
IL-6 and diabetes are often linked in research as this cytokine serves a dual role: it can either fuel inflammation or help regulate it, depending on the context.
This duality can be confusing, but in the context of type 1 diabetes, IL-6 acts more as an antagonist.
Research published in Nature Reviews Endocrinology highlights how IL-6, when elevated, contributes to beta-cell dysfunction.
For me, this meant that inflammation spurred by IL-6 was another factor driving my body to destroy its insulin-producing cells.
The connection between IL-6 diabetes responses and autoimmune activity makes this cytokine one of the key players in the development of the disease.
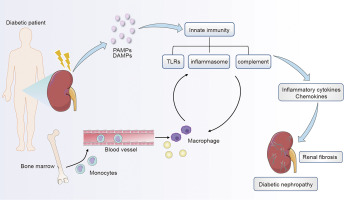
Cytokine Storms and Their Connection to Diabetes
You have likely heard the term “cytokine storm” in recent discussions around viral infections, but it is not just limited to that realm.
A cytokine storm refers to an overproduction of inflammatory cytokines, causing the immune system to go haywire.
Interestingly, there is research suggesting that cytokine storms can exacerbate diabetes.
While cytokine storm and diabetes are typically discussed in the context of acute infections, the long-term effects of repeated cytokine overproduction can worsen conditions like type 1 diabetes.
When the immune system continuously produces inflammatory cytokines, it speeds up the destruction of pancreatic beta cells, pushing people like me further into insulin dependence.
In some cases, this storm of cytokines may even accelerate the onset of diabetes in those genetically predisposed.
Daily Life Implications of Cytokine Activity in Diabetes
Living with type 1 diabetes, I have noticed how the body’s constant state of inflammation, driven by cytokines, impacts daily life.
Simple things like stress or infection such as Coxsackievirus can cause my blood sugar levels to spike, all thanks to the overactive cytokine response.
I have even had moments where inflammation from an unrelated illness seemed to make my diabetes harder to manage, which aligns with studies showing the role of inflammation in blood sugar regulation.
Medications like metformin, commonly used in type 2 diabetes, have been found to influence cytokine activity.
While not typically prescribed for type 1 diabetes, metformin and cytokines research shows that it can reduce inflammation, which might be beneficial in managing the immune response that contributes to beta-cell destruction.
Top 5 FAQs on Cytokines and Type 1 Diabetes
A quick look at the top 5 burning queries on this topic:
Q-1: Which Cytokines most Strongly Drive β-cell Injury in T1D?
The classic trio—IL-1β, TNF-α, and IFN-γ—acts synergistically. Together they raise nitric oxide, trigger ER and mitochondrial stress, and blunt insulin secretion, pushing β-cells toward dysfunction or death. This mix is the standard “cytokine cocktail” in lab models of T1D.
Q-2: What’s the Role of Type I Interferons like IFN-α?
They’re amplifiers. IFN-α heightens HLA class I on β-cells and broadens antigen presentation, making islets more “visible” to autoreactive T cells. In people at risk or newly diagnosed, type I interferon signatures show up, linking viral sensing to autoimmunity.
Q-3: Do Chemokines matter, or are they Background Noise?
They’re the traffic controllers. CXCL10 (with receptor CXCR3) is detected in T1D islets and helps recruit aggressive T cells. Work also points to an XCL1–XCR1 dendritic-cell axis that intensifies antigen presentation in autoantibody-positive individuals.
Q-4: Can Targeting Cytokine Pathways slow T1D?
Clinical signals are encouraging. Blocking IL-21 with a GLP-1 agonist has preserved β-cell function in recent-onset T1D. Low-dose IL-2 aims to expand regulatory T cells. JAK inhibition, which dampens multiple cytokine signals, has preserved C-peptide in new-onset patients.
Q-5: Are β-cells just Victims Here?
Not quite. β-cells express pattern-recognition receptors and can produce type I interferons in response to viral or danger cues. That self-defense can boost chemokines and HLA expression, escalating immune attention—one reason “β-cell-intrinsic immunity” is now a hot research area.
Are Cytokines the Hidden Culprits – My Opinion:
So, are cytokines the hidden culprits fueling type 1 diabetes?
Based on the evidence and my own experience, the answer is a resounding yes.
While many factors contribute to the onset of type 1 diabetes, cytokines undoubtedly play a significant role in driving the autoimmune attack on insulin-producing cells.
From TNF alpha in diabetes to IL-6 and cytokine storms, the influence of these proteins on inflammation and immune regulation is hard to ignore.
Summing up, cytokines are like the match that lights the autoimmune fire, gradually leading to the destruction of pancreatic beta cells.
While there is no simple solution to this complex problem, understanding the role of cytokines in diabetes opens the door to new treatment possibilities that could focus on calming the immune response.
I also regularly advocate the use of herbs that lower blood sugar fast.
In the end, acknowledging cytokines’ influence helps make sense of why type 1 diabetes behaves the way it does.
Whether through inflammation or direct immune signaling, cytokines are clearly major players in the autoimmune process that defines type 1 diabetes.
Their role in my personal experience with the disease is undeniable—and they may just be the hidden culprits we have been looking for.
References: