How Age Affects Insulin Sensitivity in Type 2 Diabetes?
- admin
- October 11, 2024
- 7:32 pm
- No Comments

As someone living with type 2 diabetes, I have often wondered why managing my blood sugar seems to become more challenging as I get older.
When I was first diagnosed, maintaining healthy blood sugar levels through diet and exercise felt more straightforward.
But as the years passed, I noticed subtle changes—my body did not respond to the same strategies as effectively as before. I realized that age, alongside lifestyle factors, plays a critical role in insulin sensitivity.
Insulin sensitivity is key to managing type 2 diabetes because it determines how well the body responds to insulin, the hormone responsible for regulating blood glucose.
When insulin sensitivity decreases, the body requires more insulin to keep blood sugar in check, and this is where the trouble begins for many people as they age.
In this article, we shall explore how age affects insulin sensitivity in type 2 diabetes, diving into the physiological changes, lifestyle challenges, and scientific research behind it.
If you are wondering why managing diabetes seems to get trickier with time, you’re in the right place.
Points Covered in this Article:
- Understanding Insulin Sensitivity in Type 2 Diabetes
- How Aging Affects Insulin Production and Usage
- The Impact of Muscle Mass Loss on Insulin Sensitivity
- How Hormonal Changes with Age Affect Insulin Sensitivity
- The Role of Physical Activity in Maintaining Insulin Sensitivity in Older Adults
- The Connection Between Age-Related Inflammation and Insulin Resistance
- Real-Life Examples: Age-Related Insulin Sensitivity Changes in Daily Life
- Conclusion: How Age Affects Insulin Sensitivity in Type 2 Diabetes
Understanding Insulin Sensitivity in Type 2 Diabetes
Insulin sensitivity refers to how responsive the body’s cells are to insulin.
In people without diabetes, insulin helps glucose from the bloodstream enter cells, where it is used for energy. However, in type 2 diabetes, the body becomes resistant to insulin.
This means that more insulin is needed to get glucose into the cells, and when the pancreas can’t keep up, blood sugar levels rise.
As we age, this natural decline in insulin sensitivity can worsen, making it harder to manage blood sugar.
But what exactly happens as we grow older that affects insulin sensitivity so drastically?
It turns out that several factors, both physiological and lifestyle-related, contribute to this decline.
How Aging Affects Insulin Production and Usage?
One of the biggest ways aging affects insulin sensitivity is through changes in how the pancreas produces and secretes insulin.
As we age, the pancreas may become less efficient at producing insulin, and the body’s cells also become less responsive to it. This combination leads to higher blood sugar levels.
A study published in The Journal of Clinical Endocrinology & Metabolism found that insulin sensitivity declines with age, particularly after the age of 40.
This decline is partly due to the reduced function of beta cells in the pancreas, which are responsible for insulin production.
In my personal experience, I have noticed that my blood sugar tends to spike more easily after meals, even if I haven’t changed my eating habits.
This suggests that my body isn’t using insulin as efficiently as it once did, a common occurrence as we age.
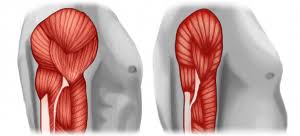
The Impact of Muscle Mass Loss on Insulin Sensitivity
Muscle is more than just strength and aesthetics—it is one of the body’s most insulin-sensitive tissues. As we age, we naturally lose muscle mass in a process called sarcopenia, and with it, our metabolic efficiency takes a hit.
Why?
Because skeletal muscle plays a key role in glucose disposal. When you eat carbohydrates, insulin helps shuttle glucose from your bloodstream into your muscles for storage or fuel. Less muscle means fewer places for glucose to go, resulting in elevated blood sugar and insulin resistance.
Studies show that muscle accounts for nearly 80% of post-meal glucose uptake. So when muscle mass declines, insulin has a harder time doing its job. This becomes a critical issue in people over 50, particularly those living with type 2 diabetes or prediabetes.
For example, a 2022 study in The Journal of Clinical Endocrinology & Metabolism found that adults with lower muscle mass had significantly poorer insulin sensitivity—even when body fat was similar. This shows that it’s not just about fat gain but also muscle loss.
A sedentary lifestyle accelerates sarcopenia. Sitting for long hours, avoiding resistance training, and poor nutrition (especially low protein intake) compound the problem.
But the good news? It is reversible.
Regular strength training controls blood sugar levels—even just 2–3 times a week—has been shown to improve insulin sensitivity by increasing GLUT4 transporters in muscle cells, which help usher glucose into cells more efficiently.
Personally, I have found that even modest gains in muscle tone from weight training helped flatten my post-meal glucose spikes.
Something as simple as squats, resistance bands, taking a brisk walk, carrying groceries with intention can build muscle.
Bottom line: keeping your muscles strong is not just for mobility—it’s a frontline defense against insulin resistance.
Whether you are 30 or 70, your biceps might just be your best bet against blood sugar chaos.
How Hormonal Changes with Age Affect Insulin? Sensitivity?
As we age, hormonal changes also come into play.
For instance, hormones like growth hormone and testosterone, which help regulate metabolism and muscle mass, decline with age.
Lower levels of these hormones can reduce insulin sensitivity and make blood sugar regulation more difficult.
In women, menopause brings hormonal shifts that can affect how the body handles insulin.
The decline in estrogen levels during menopause has been shown to decrease insulin sensitivity, making blood sugar management more challenging for postmenopausal women with type 2 diabetes.
A study published in Diabetes Care suggests that postmenopausal women are at a higher risk of insulin resistance, further complicating diabetes management.
This shift in hormones also impacted my daily routine.
I had to make adjustments to both my exercise regimen and diet to compensate for these hormonal changes, especially after reaching my 50s.
The Role of Physical Activity in Maintaining Insulin Sensitivity in Older Adults
Physical activity plays a crucial role in maintaining insulin sensitivity, particularly as we age.
Regular exercise helps keep muscles active and enhances their ability to absorb glucose, which improves insulin sensitivity.
In older adults, staying active can offset some of the age-related declines in muscle mass and hormone levels.
Aerobic exercise, such as walking or swimming, helps the body use insulin more efficiently, while strength training increases muscle mass and boosts metabolism.
According to the National Institutes of Health, regular physical activity is one of the most effective ways to combat insulin resistance and maintain glycemic control.
From personal experience, I found that as I got older, I couldn’t rely solely on diet to manage my blood sugar. Incorporating regular exercise into my routine became essential to maintaining stable blood sugar levels and overall health.
The Connection Between Age-Related Inflammation and Insulin Resistance
Inflammation is another factor that affects insulin sensitivity as we age. Chronic low-grade inflammation, often referred to as “inflammaging,” increases as we get older.
This type of inflammation has been linked to insulin resistance, making it harder for the body to manage blood sugar effectively.
Studies have shown that chronic inflammation can interfere with insulin signaling pathways, making cells less responsive to insulin.
A study published in The Lancet Diabetes & Endocrinology found that inflammation is a key driver of age-related insulin resistance.
In my own life, I noticed that periods of poor sleep or high stress—both of which can increase inflammation—made it much harder to control my blood sugar.
This connection between inflammation and insulin resistance became more apparent as I got older.
Real-Life Examples: Age-Related Insulin Sensitivity Changes in Daily Life
As someone who has lived with type 2 diabetes for over a decade, I have experienced firsthand how aging affects insulin sensitivity.
In my 40s, I could control my blood sugar with relative ease through diet, supplements to lower blood sugar and moderate exercise. But once I hit my 50s, I noticed that my body’s response to the same strategies wasn’t as effective.
For instance, a meal that previously resulted in a modest blood sugar rise would now cause a significant spike.
I also found that my body took longer to recover after meals, which led to higher fasting blood sugar levels the next morning.
These changes were not the result of poor management—they were a natural part of aging that required me to adjust my approach.
My Take on How Age Affects Insulin Sensitivity in Type 2 Diabetes
To answer the question, “How does age affect insulin sensitivity in type 2 diabetes?” the answer is multifaceted.
As we age, several physiological factors come into play: reduced insulin production, muscle mass loss, hormonal changes, and increased inflammation.
All of these factors contribute to a decline in insulin sensitivity, making blood sugar management more challenging.
However, understanding these changes is the first step toward managing them.
While aging may reduce insulin sensitivity, adopting strategies like regular physical activity, strength training, and anti-inflammatory diets can help mitigate some of these effects.
Although the challenges of managing type 2 diabetes may increase with age, they can be addressed with awareness, consistency, and proactive management via diabetes support groups.
References: