How Abdominal Trauma Leads to Pancreatic Damage and Diabetes?
- admin
- November 5, 2024
- 4:49 pm
- No Comments
Your pancreas is that sneaky little organ nestled behind your stomach, often overlooked until something goes horribly wrong.
Today, bestdietarysupplementfordiabetics shall be diving into the world of abdominal trauma and exploring how an injury to your midsection can damage this delicate gland, leading to complications like type 3c diabetes.
If you have ever wondered why a swift punch to the gut or a car accident can have such serious ramifications, you have come to the right place.
Article Contents:
- What is Abdominal Trauma?
- How the Pancreas Works
- Mechanism of Pancreatic Damage from Trauma
- Types of Pancreatic Injuries
- How Pancreatic Damage Affects Insulin Production
- Why Pancreatic Damage Can Lead to Type 3c Diabetes
- Real-Life Examples: Stories of Trauma and Type 3c Diabetes
- FAQs on Pancreatic Tumor & Type 3c Diabetes
- Scientific Evidence Linking Trauma to Diabetes
What is Abdominal Trauma?
Let’s start with the basics.
Abdominal trauma refers to any injury to the abdomen caused by blunt force (like a car accident or a fall) or penetrating trauma (think stabbing or a gunshot).
The pancreas, unfortunately, often becomes collateral damage in these situations.
Since it lies deep within the abdomen, sandwiched between other organs, it is susceptible to both direct and indirect trauma.
According to the Journal of Trauma and Acute Care Surgery, abdominal trauma accounts for a significant number of hospital admissions and is one of the leading causes of organ damage.
How the Pancreas Works?
To understand the chaos that trauma can unleash on your pancreas, it is important to know what this organ does.
The pancreas is a dual-purpose gland.
It plays a role in digestion by secreting enzymes and regulates blood sugar levels by producing insulin and glucagon.
It is like the Swiss Army knife of your digestive system.
When the pancreas is injured, these functions can go haywire, setting the stage for serious metabolic issues.
Mechanism of Pancreatic Damage from Trauma
So, how does trauma damage the pancreas?
Well, abdominal trauma can cause the pancreas to become bruised, lacerated, or even completely crushed.
The American Journal of Surgery explains that the pancreas’s location makes it vulnerable to compression against the spine during blunt force impact.
When the pancreas is injured, its cells may release digestive enzymes internally, which can lead to a condition called pancreatitis.
Imagine a kitchen blender breaking and spilling its contents everywhere.
Not good, right?
Types of Pancreatic Injuries
Pancreatic injuries can range from mild contusions to severe lacerations.
According to Pancreatology, there are generally four types:
- Contusions and Minor Tears: Often go unnoticed but can still cause internal inflammation.
- Severe Lacerations: Can disrupt the organ’s ability to produce insulin.
- Complete Transection: A rare but catastrophic injury where the pancreas is essentially cut in half.
- Crushing Injuries: Typically occur in high-impact accidents and have serious consequences.
How Pancreatic Damage Affects Insulin Production?
Here is where things get dicey.
The pancreas has specialized cells called islets of Langerhans that produce insulin.
Damage to the pancreas can destroy these cells, disrupting insulin production and leading to high blood sugar levels.
A study published in Diabetes Care found that even partial damage to the pancreas can significantly impact glucose regulation.
And because the pancreas does not regenerate like the liver, any damage is usually permanent.
Why Pancreatic Damage Can Lead to Type 3c Diabetes?
You have probably heard of type 1 and type 2 diabetes, but type 3c is a different beast.
It is a form of diabetes that occurs specifically due to damage or disease in the pancreas.
Unlike type 1 or type 2, which are linked to autoimmune and insulin resistance issues respectively, type 3c is directly caused by the organ’s inability to function.
According to research published in Pancreas Journal, up to 10% of all diabetes cases may actually be type 3c, yet it is frequently misdiagnosed.
Abdominal trauma is a key culprit, disrupting both the endocrine and exocrine functions of the pancreas.
>>> Want to Learn How I “Treated My Damaged Pancreas Naturally” & “Reversed My Type 2 Diabetes” at Home??? Click Here to Find Out! <<<
Real-Life Examples: Stories of Trauma and Type 3c Diabetes
Take John, for instance, a 35-year-old construction worker who experienced a severe fall on the job.
After landing abdomen-first onto a steel beam, he was rushed to the hospital.
Though he initially recovered, John began experiencing symptoms like extreme thirst and fatigue months later.
Turns out, his pancreas had suffered severe damage, and he was eventually diagnosed with type 3c diabetes.
Or consider Sarah, who was in a car accident.
The seatbelt, while saving her life, caused blunt force trauma to her abdomen.
Her pancreas developed chronic pancreatitis, and within a year, she struggled with high blood sugar, leading to a type 3c diabetes diagnosis.
This is when Sarah had to rely on natural methods to control her blood sugar levels.
Scientific Evidence Linking Trauma to Diabetes
There is a wealth of scientific literature connecting pancreatic trauma to diabetes.
A study in the Journal of Gastrointestinal Surgery highlights that 40% of patients with severe pancreatic injury develop some form of diabetes.
Another study from Endocrine Connections explains the biochemical cascade that occurs, including the release of inflammatory cytokines that further damage pancreatic cells.
Additionally, research from Trauma Surgery & Acute Care Open emphasizes that timely intervention can sometimes mitigate the risk, but in many cases, the damage is done before symptoms even appear.
FAQs on Pancreatic Tumor & Type 3c Diabetes
Q-1: How does a single abdominal blow turn into long-term pancreatic injury and diabetes months later?
A-1: A hard impact (crash, handlebar, contact sport) can bruise or lacerate the pancreas and kink the main duct. Even when pain settles, tiny leaks of enzyme-rich fluid and low-grade inflammation can persist.
As the area heals, scar tissue narrows ducts and starves downstream tissue of enzyme flow, while nearby islets lose blood supply. Over weeks to months, this “slow scarring” converts a one-time injury into chronic exocrine insufficiency and progressive loss of insulin/glucagon output—classic Type 3c physiology.
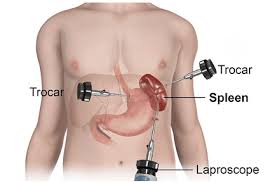
Q-2: Why does trauma near the spleen carry a special diabetes risk?
A-2: The insulin-producing islets cluster densely in the pancreatic tail, which sits by the spleen. Blunt trauma or surgery for splenic injury can unintentionally damage or remove tail tissue.
Losing that real estate trims β-cell mass directly, so even modest post-injury inflammation can tip someone from normal glucose to post-meal highs and, later, fasting abnormalities.
Q-3: What’s the difference between early “stress hyperglycemia” after trauma and later Type 3c diabetes?
A-3: Right after injury, stress hormones (adrenaline, cortisol) push glucose up—even with a normal pancreas. That surge usually fades as the body recovers.
Type 3c diabetes emerges later and behaves differently: erratic post-meal spikes, greasy stools from fat maldigestion, and surprising late lows due to weak glucagon. If high sugars are still present weeks to months later—especially with digestive changes—think structural pancreatic damage, not just stress.
Q-4: Can trauma surgery itself nudge someone toward diabetes?
A-4: Yes. Repairs for duct injuries, debridement of dead tissue, or partial pancreatectomy save lives but reduce functional islet mass and alter duct anatomy.
Afterward, fat and starch may digest poorly (dampening incretin signals) while insulin reserve is smaller. The combination raises post-meal glucose and makes dosing less predictable unless enzymes are replaced and meals are structured.
Q-5: What day-to-day steps help when post-trauma pancreas reserve is limited?
A-5: Make digestion efficient to steady glucose appearance: take pancreatic enzymes with the first bite and match dose to meal fat; use smaller, protein-anchored meals; and limit alcohol (which blunts liver glucose release and can trigger lows).
Track patterns with a meter/CGM—especially overnight—because counter-regulation is weaker. If the spleen was removed, keep vaccinations current and discuss infection plans; systemic infections can destabilize glucose in a pancreas already running on reserve.
The Domino Effect of Pancreatic Trauma
In summary, abdominal trauma is more than just a temporary inconvenience.
It can have long-lasting effects, particularly on your pancreas.
When this crucial organ is compromised, the risk of developing type 3c diabetes increases.
Understanding the link between trauma and pancreatic dysfunction can help raise awareness and improve diagnosis rates.
And while we are not here to offer solutions today, one thing is clear: protecting your midsection is more important than you might think.
So, the next time you buckle up or engage in a high-risk activity, remember your pancreas is counting on you!
References: