How Mitochondrial Dysfunction in Optic Atrophy Affects Beta-Cell Energy Production?
- admin
- January 3, 2025
- 5:13 pm
- No Comments
Mitochondria are often called the “powerhouses of the cell,” and for good reason—they are responsible for producing ATP, the energy currency necessary for various cellular functions.
In conditions like optic atrophy, where mitochondrial function is compromised, the ripple effects extend far beyond vision.
This article by bestdietarysupplementfordiabetics.com explores how mitochondrial dysfunction in optic atrophy disrupts beta-cell energy production, contributing to impaired insulin secretion and glucose regulation.
We will analyze the mechanisms behind this connection, delve into the biological processes affected, and discuss real-life case studies to provide a comprehensive understanding.
Index
- Introduction to Mitochondrial Dysfunction in Optic Atrophy
- The Role of Mitochondria in Beta-Cell Function
- Mechanisms Linking Mitochondrial Dysfunction and Beta-Cell Impairment
- ATP Production and Insulin Secretion
- Oxidative Stress and Beta-Cell Damage
- Case Studies Highlighting the Impact
- Case Study 1: Sarah’s Dual Diagnosis of Optic Atrophy and Diabetes
- Case Study 2: Mark’s Struggle with Energy Deficits
- Scientific Evidence Supporting the Connection
- FAQs on Mitochondrial Dysfunction in Optic Atrophy
- Conclusion
Introduction to Mitochondrial Dysfunction in Optic Atrophy
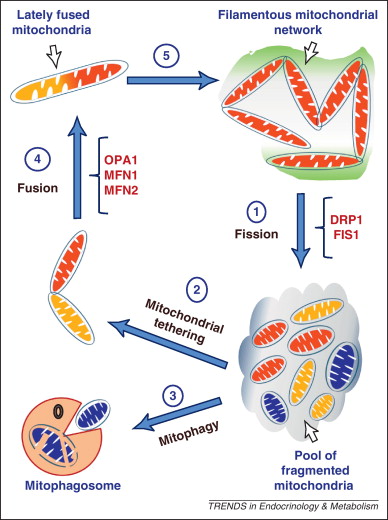
Optic atrophy, a condition marked by the degeneration of optic nerve fibers, stems primarily from mitochondrial dysfunction. Mutations in genes like OPA1 are at the heart of this issue, disrupting mitochondrial dynamics, fusion processes, and ATP production.
While optic atrophy is widely recognized for its impact on vision, its systemic effects extend far beyond the eyes, often influencing other energy-dependent tissues such as pancreatic beta-cells. These beta-cells rely heavily on mitochondrial energy production to regulate insulin secretion, and any disruption can lead to significant metabolic consequences.
Mitochondrial dysfunction impairs glucose-stimulated insulin secretion by reducing ATP availability and increasing oxidative stress, compromising glucose regulation.
This article explores the intricate relationship between optic atrophy and beta-cell energy deficits, delving into how mitochondrial dysfunction in this condition influences systemic glucose metabolism.
By connecting the dots between these seemingly distinct domains, we aim to shed light on an overlooked aspect of this genetic disorder.
The Role of Mitochondria in Beta-Cell Function
Beta-cells, housed within the islets of Langerhans in the pancreas, are vital for insulin production and secretion, a process directly tied to rising blood glucose levels. This function is profoundly energy-dependent, with mitochondria playing a central role in ATP production.
ATP acts as a critical signaling molecule, triggering the closure of KATP channels in the beta-cell membrane. This event initiates membrane depolarization, allowing calcium influx through voltage-gated calcium channels, ultimately driving the exocytosis of insulin granules.
Beyond energy production, mitochondria are integral to beta-cell health, managing oxidative stress and orchestrating key cell signaling pathways.
Impairments in these mitochondrial functions—such as those caused by OPA1 mutations linked to optic atrophy—compromise the beta-cell’s ability to maintain glucose homeostasis.
Scientific evidence underscores this link. A study published in Diabetes (Maechler & Wollheim, 2001) revealed that mitochondrial dysfunction in beta-cells significantly reduces ATP generation, impairing insulin secretion. Similarly, research by Del Prato et al. (2002) highlighted how oxidative stress due to mitochondrial defects exacerbates beta-cell apoptosis, further undermining glucose regulation.
These findings emphasize how mitochondrial dysfunction, as seen in optic atrophy, creates a ripple effect that disrupts systemic glucose metabolism, illustrating the critical need to address mitochondrial health in managing such conditions.
Mechanisms Linking Mitochondrial Dysfunction and Beta-Cell Impairment
A quick look at these:
ATP Production and Insulin Secretion
Mitochondria generate ATP through oxidative phosphorylation, a process that becomes inefficient in the presence of mitochondrial dysfunction. Reduced ATP availability hinders the energy-dependent steps of insulin secretion, leaving beta-cells unable to meet metabolic demands.
A study published in Nature Genetics (Zorzano et al., 2010) demonstrated that OPA1 mutations impair mitochondrial cristae structure, reducing ATP synthesis. This directly affects the glucose-stimulated insulin secretion pathway in beta-cells, leading to hyperglycemia.
Oxidative Stress and Beta-Cell Damage
Dysfunctional mitochondria are major sources of reactive oxygen species (ROS). Elevated ROS levels cause oxidative stress, damaging beta-cell DNA, proteins, and lipids.
Beta-cells are particularly vulnerable to oxidative stress due to their low antioxidant capacity. Chronic oxidative stress exacerbates mitochondrial dysfunction, creating a vicious cycle that further impairs insulin secretion.
Research in Diabetes (Sivitz & Yorek, 2010) highlighted that oxidative stress in beta-cells correlates with reduced insulin secretion and increased apoptosis, emphasizing its role in diabetes pathophysiology.
Sarah’s Journey with Optic Atrophy and Glucose Dysregulation
Sarah, a 34-year-old teacher, was diagnosed with optic atrophy caused by OPA1 mutations.
Over time, she began experiencing persistent symptoms of diabetes, including excessive thirst and frequent urination.
Medical evaluations revealed mitochondrial dysfunction not only in her optic nerve but also in her pancreatic beta-cells, leading to impaired insulin secretion.
Her treatment plan incorporated glucose-lowering medications alongside interventions aimed at supporting mitochondrial health, such as antioxidants.
Through a tailored approach, Sarah improved her glucose control and maintained her quality of life, despite the challenges posed by her dual diagnosis.
Mark’s Experience with Vision Loss and Metabolic Imbalances
Mark, a 40-year-old athlete, noticed progressive vision deterioration accompanied by unexplained fatigue and elevated fasting glucose levels.
Testing identified optic atrophy and revealed that mitochondrial dysfunction extended beyond his optic nerve, affecting energy production in his beta-cells.
This resulted in inadequate insulin secretion and poor glucose regulation.
A combination of lifestyle adjustments, including a nutrient-rich diet to support mitochondrial function, and glucose monitoring significantly improved Mark’s metabolic health and physical performance.
These examples highlight the systemic impact of mitochondrial dysfunction in optic atrophy, showcasing its role in disrupting energy production across critical tissues, including beta-cells.
Scientific Evidence Supporting the Connection
Study 1: Zorzano et al., 2010 (Nature Genetics)
This study demonstrated that mutations in OPA1 disrupt mitochondrial cristae, reducing ATP synthesis and impairing beta-cell function.
Study 2: Sivitz & Yorek, 2010 (Diabetes)
Highlighted the role of oxidative stress in beta-cell apoptosis and its impact on insulin secretion in conditions associated with mitochondrial dysfunction.
Study 3: Pospisilik et al., 2007 (Cell Metabolism)
Explored how mitochondrial dysfunction affects glucose homeostasis, emphasizing its systemic effects beyond optic atrophy.
Study 4: Del Prato et al., 2002 (Diabetologia)
Confirmed the link between mitochondrial energy deficits and impaired glucose-stimulated insulin secretion in beta-cells.
FAQs on Mitochondrial Dysfunction in Optic Atrophy
Q-1: How does mitochondrial dysfunction in optic atrophy impact beta-cell energy production?
A-1: Mitochondrial dysfunction in optic atrophy, often caused by genetic mutations affecting mitochondrial dynamics, disrupts the structure and function of mitochondria. This disruption leads to reduced ATP production and impaired regulation of cell survival, which may compromise energy generation in beta-cells, essential for insulin secretion and glucose regulation.
Q-2: Are beta-cells particularly vulnerable to mitochondrial dysfunction seen in optic atrophy?
A-2: Yes, beta-cells rely heavily on mitochondrial energy production to function properly. Although optic atrophy primarily affects nerve cells in the eye, the systemic nature of mitochondrial dysfunction can make beta-cells susceptible to impaired energy metabolism, potentially affecting their ability to produce and release insulin efficiently.
Q-3: What cellular mechanisms link mitochondrial dysfunction in optic atrophy to beta-cell impairment?
A-3: Key mechanisms include increased oxidative stress from excess reactive oxygen species and disturbed calcium signaling within cells. Both factors can damage beta-cell mitochondria, reducing energy output and disrupting insulin secretion, which may contribute to metabolic imbalances.
Q-4: Can therapies targeting mitochondrial health in optic atrophy improve beta-cell energy production?
A-4: Therapeutic approaches that enhance mitochondrial fusion, reduce oxidative damage, or improve mitochondrial biogenesis have shown promise in restoring mitochondrial function. While primarily aimed at neural cells, these therapies may also support beta-cell energy metabolism, potentially improving their functional capacity.
Q-5: Is there a connection between optic atrophy and metabolic disorders affecting beta-cell function?
A-5: Although optic atrophy is mainly linked to visual deficits from nerve cell damage, the underlying mitochondrial dysfunction could influence systemic metabolic processes. This suggests a possible but not yet well-defined link between optic atrophy and metabolic conditions involving beta-cell dysfunction, warranting further research.
Conclusion
Mitochondrial dysfunction in optic atrophy, often associated with mutations in genes such as OPA1, has far-reaching effects beyond vision loss, significantly impairing pancreatic beta-cell function.
Beta-cells rely heavily on mitochondria for ATP production, a critical process for insulin secretion. Disrupted mitochondrial dynamics in optic atrophy reduce ATP availability, impairing the closure of KATP channels, membrane depolarization, and insulin granule release.
Additionally, increased oxidative stress caused by mitochondrial dysfunction damages beta-cell membranes and proteins, further compromising glucose regulation.
This systemic impact links optic atrophy to metabolic disorders, such as type 1 diabetes, emphasizing the need for integrated care.
A study in Diabetes (Rutter et al., 2010) highlighted the role of oxidative stress in beta-cell failure, reinforcing the connection between mitochondrial health and glucose homeostasis.
Advances in mitochondrial research offer new therapeutic avenues, from antioxidant treatments to gene-targeted interventions, aiming to improve outcomes for those affected by both optic atrophy and associated metabolic challenges.
References: