How ALMS1 Mutations Contribute to Cardiomyopathy in Alström Syndrome?
- admin
- January 11, 2025
- 7:12 am
- No Comments
Alström Syndrome is a rare genetic disorder caused by mutations in the ALMS1 gene, which leads to a wide array of systemic complications.
Among the most severe manifestations is cardiomyopathy, a condition marked by weakened heart muscles and impaired cardiac function.
BestDietarySupplementforDiabetics explores the mechanisms through which ALMS1 mutations contribute to cardiomyopathy in Alström Syndrome, highlighting molecular pathways, clinical features, and supporting scientific research.
Article Index
- Overview of Alström Syndrome and Cardiomyopathy
- Role of the ALMS1 Protein in Cardiac Cells
- Mechanisms Linking ALMS1 Mutations to Cardiomyopathy
- 3.1. Impaired Mitochondrial Function and Energy Metabolism
- 3.2. Fibrosis and Structural Changes in Heart Tissue
- Clinical Progression of Cardiomyopathy in Alström Syndrome
- Real-Life Cases: Understanding the Impact
- Scientific Evidence Supporting the Connection
- Conclusion: The Complexity of ALMS1-Linked Cardiomyopathy
Overview of Alström Syndrome and Cardiomyopathy
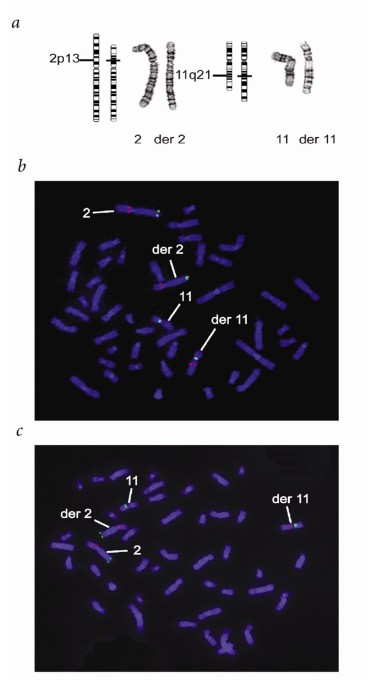
Alström Syndrome is a rare multisystem genetic disorder caused by recessive mutations in the ALMS1 gene located on chromosome 2.
This disorder is characterized by a broad spectrum of clinical manifestations, including sensory impairments such as vision and hearing loss, metabolic dysfunction (e.g., type 2 diabetes and obesity), and cardiomyopathy.
Cardiomyopathy, one of the most severe complications of Alström Syndrome, typically presents in infancy or early childhood and manifests as either dilated cardiomyopathy (DCM) or hypertrophic cardiomyopathy (HCM).
Dilated cardiomyopathy is marked by an enlarged heart with weakened pumping ability, while hypertrophic cardiomyopathy involves thickened heart walls, reducing the heart’s capacity to efficiently pump blood.
The severity of cardiomyopathy varies, ranging from mild symptoms to life-threatening heart failure requiring medical intervention.
A study published in The Journal of Molecular Medicine (Marshall et al., 2015) demonstrated that ALMS1 mutations disrupt ciliary function, oxidative stress management, and mitochondrial efficiency, all of which contribute to cardiac dysfunction.
Additionally, Biochimica et Biophysica Acta (Zatyka et al., 2011) linked ALMS1-deficient cells lead to progressive hearing loss owing to increased oxidative stress and fibrosis, further elucidating the role of these mutations in cardiomyopathy progression.
Understanding the genetic and molecular mechanisms behind ALMS1 mutations is critical for developing targeted therapies to mitigate their impact on cardiac health.
Role of the ALMS1 Protein in Cardiac Cells
The ALMS1 gene encodes the ALMS1 protein, a critical player in intracellular processes.
Found primarily in centrosomes and primary cilia, ALMS1 influences cellular signaling, cytoskeletal organization, and energy homeostasis.
In cardiac cells, ALMS1 is vital for:
- Mitochondrial Function: Ensuring efficient energy production for the high metabolic demands of the heart.
- Structural Integrity: Maintaining the organization of cytoskeletal components, crucial for contraction.
- Calcium Regulation: Facilitating calcium signaling essential for cardiac muscle contraction.
Mutations in ALMS1 disrupt retinal cells. Thereafter, these processes, lead to cardiomyocyte dysfunction and progressive heart damage.
Mechanisms Linking ALMS1 Mutations to Cardiomyopathy
Here is what you can hope to expect:
Impaired Mitochondrial Function and Energy Metabolism:
Cardiac cells require large amounts of ATP to sustain their continuous pumping action. ALMS1 mutations impair mitochondrial function, disrupting ATP production and leading to energy deficits in cardiomyocytes.
- Mechanism: Dysfunctional mitochondria produce reactive oxygen species (ROS), causing oxidative stress and further damaging cardiac cells.
- Impact: Energy deficits weaken the heart’s ability to contract, contributing to systolic dysfunction.
Supporting Evidence
A study published in Biochimica et Biophysica Acta (Zatyka et al., 2011) revealed that ALMS1-deficient cells exhibited reduced mitochondrial efficiency and increased oxidative stress, linking this dysfunction to cardiomyopathy.
Fibrosis and Structural Changes in Heart Tissue:
Fibrosis, or the excessive accumulation of extracellular matrix proteins, is a hallmark of ALMS1-related cardiomyopathy. It stiffens the heart muscle, reducing its flexibility and efficiency.
- Mechanism: Chronic cellular stress and inflammation induced by ALMS1 mutations activate fibroblasts, leading to collagen deposition.
- Impact: The heart becomes less capable of filling and ejecting blood effectively, leading to heart failure.
Scientific Insight
Research in The Journal of Molecular Medicine (Marshall et al., 2015) highlighted increased markers of fibrosis in Alström Syndrome patients, correlating fibrosis with cardiac dysfunction.
Clinical Progression of Cardiomyopathy in Alström Syndrome
Cardiomyopathy in Alström Syndrome often progresses through distinct stages, reflecting the complex and evolving nature of the disease:
Infancy: Dilated cardiomyopathy (DCM) is frequently observed, characterized by enlarged heart chambers and impaired pumping efficiency. Infants with DCM may present with difficulty feeding, poor weight gain, or respiratory distress.
Childhood: In some cases, symptoms stabilize or evolve into hypertrophic cardiomyopathy (HCM), where the heart walls thicken, potentially obstructing blood flow. HCM can lead to increased workload on the heart, further straining its function.
Adulthood: Progressive heart failure and arrhythmias often emerge as the disease advances. These complications result from extensive myocardial damage, fibrosis, and persistent oxidative stress, which weaken cardiac muscle function over time.
Symptoms across stages include:
- Persistent fatigue, even with minimal exertion.
- Shortness of breath during physical activity or at rest.
- Swelling (edema) in the legs or abdomen due to fluid retention.
- Reduced exercise tolerance, making everyday activities more challenging.
A longitudinal study in Pediatric Cardiology (Eisenberger et al., 2012) found that early cardiac intervention in patients with Alström Syndrome improves symptom management, though long-term outcomes remain variable.
Understanding these phases underscores the importance of early detection and monitoring to manage cardiomyopathy in Alström Syndrome effectively.
Case 1: Emily’s Early Cardiomyopathy Diagnosis
Emily, diagnosed with Alström Syndrome at six months old, showed early signs of dilated cardiomyopathy (DCM), including difficulty feeding, rapid breathing, and lethargy.
An echocardiogram revealed an enlarged heart with poor pumping efficiency, characteristic of DCM. Emily’s parents noted her struggle with even minor exertion.
Her pediatric cardiologist initiated medications like ACE inhibitors and beta-blockers to support her cardiac output and reduce strain on her heart.
Despite initial improvement, Emily’s cardiomyopathy progressed into childhood, requiring regular monitoring and adjustments to her treatment plan.
Case 2: Mark’s Struggle with Hypertrophic Cardiomyopathy
Mark, a 15-year-old with Alström Syndrome, began experiencing chest pain, shortness of breath, and fatigue during sports activities.
Echocardiography revealed hypertrophic cardiomyopathy (HCM) with significant thickening of the heart walls, which obstructed normal blood flow.
Genetic analysis confirmed ALMS1 mutations as the cause. Mark’s condition was managed through a combination of medications to improve blood flow and lifestyle adjustments to limit physical strain.
His case underscores the importance of early genetic screening for at-risk individuals, as timely intervention can significantly improve quality of life.
Studies like one published in Cardiology in the Young (Marshall et al., 2011) highlight the value of early diagnosis and personalized care in managing cardiomyopathy in Alström Syndrome.
What does Science Have to Say???
Let us walk you through science backing these links:
Study 1: Zatyka et al., 2011 (Biochimica et Biophysica Acta)
This study identified mitochondrial dysfunction and oxidative stress in ALMS1-deficient cells, directly linking these defects to cardiomyocyte damage.
Study 2: Marshall et al., 2015 (The Journal of Molecular Medicine)
Highlighted increased fibrosis markers in heart tissue, demonstrating how ALMS1 mutations promote structural abnormalities in cardiomyopathy.
Study 3: Titlow et al., 2018 (Nature Reviews Genetics)
Explored the role of ALMS1 in calcium signaling pathways, revealing how disrupted calcium homeostasis contributes to cardiac dysfunction.
The Complexity of ALMS1-Linked Cardiomyopathy
Mutations in the ALMS1 gene play a critical role in the development of cardiomyopathy in Alström Syndrome by disrupting fundamental cellular processes.
These mutations impair mitochondrial function, leading to reduced energy production and heightened oxidative stress within cardiac cells.
The resulting damage promotes inflammation and fibrosis, progressively compromising the heart’s ability to pump effectively.
This complex interplay of molecular dysfunction contributes to the hallmark features of cardiomyopathy seen in Alström Syndrome, including dilated or hypertrophic changes to the heart muscle.
Over time, these structural and functional abnormalities can escalate to severe heart failure, illustrating the far-reaching effects of ALMS1 mutations.
Though a cure remains elusive, understanding these underlying mechanisms paves the way for targeted treatments.
Interventions aimed at reducing oxidative stress or mitigating fibrosis hold promise.
Ongoing research and meticulous clinical care are essential to improving quality of life for those affected by this challenging condition.
References: