Are Infections the Hidden Trigger Behind Type 1 Diabetes?
- admin
- October 1, 2024
- 5:48 pm
- No Comments

When it comes to Type 1 diabetes, the discussion often revolves around genetics and autoimmune responses, but what if there’s more to the story?
Emerging research suggests that infections, including viral, bacterial, and fungal, may play a more significant role in triggering Type 1 diabetes than we previously thought.
In this article, we will dive deep into the latest findings, explore how various infections may contribute to the onset of Type 1 diabetes, and examine what this means for those living with the condition.
Could infections be the hidden trigger behind Type 1 diabetes?
Let’s find out.
Article Index:
- Introduction to the Infection-Diabetes Link
- How Infections May Trigger Type 1 Diabetes
- Viral Infections: The Suspected Culprit Behind Type 1 Diabetes
- The Role of Bacterial and Fungal Infections in Type 1 Diabetes
- Flu, Shingles, and Diabetes: What We Know So Far
- Prevention and Management: Protecting Yourself from Infections
- Conclusion: Are Infections the Hidden Trigger Behind Type 1 Diabetes?
Introduction to the Infection-Diabetes Link
Type 1 diabetes has long been typecast as a purely autoimmune villain—with genetics holding the smoking gun and the immune system pulling the trigger.
But recently, a new suspect has entered the crime scene: infection. More specifically, viral infections may be playing a leading role in setting off the autoimmune chain reaction that results in Type 1 diabetes.
Studies now show that certain viruses—particularly enteroviruses like Coxsackie B—could be the molecular match that lights the inflammatory fire.
According to research published in Diabetologia, children with recent enterovirus infections showed a significantly higher risk of developing islet autoantibodies, the early markers of Type 1 diabetes.
It is like the immune system mistakes virus-infected beta cells or cytokines as enemy agents and never stops attacking—even after the infection clears.
Researchers at the University of Tampere in Finland further support this, suggesting that chronic or repeated exposure to these viruses could keep the immune system on high alert, tipping it into full autoimmune overdrive.
So, what if we could vaccinate against these viruses?
That is no longer science fiction. Ongoing clinical trials are investigating whether vaccines against enteroviruses might delay or even prevent Type 1 diabetes onset.
In short, while genes load the gun and autoimmunity pulls the trigger, infections may be the itchy finger on that trigger.
Understanding this infectious twist might unlock preventative strategies—and offer a fighting chance against this lifelong disease.
How Infections May Trigger Type 1 Diabetes?
Infections, especially during early life, can sometimes act as a catalyst for the onset of Type 1 diabetes. This autoimmune condition occurs when the immune system mistakenly attacks insulin-producing beta cells in the pancreas.
But how exactly do infections tip the balance?
Here is a pointwise breakdown backed by research and examples:
Molecular Mimicry Misfires:
Some viruses have proteins that closely resemble those found on pancreatic beta cells. The immune system, trying to eliminate the virus, may accidentally attack the pancreas too. Coxsackievirus B is a well-known example, often linked to such mistaken identity.Enterovirus Exposure in Early Life
Data from the TEDDY study showed a significant link between enterovirus infections in infancy and the development of islet autoantibodies—early markers of Type 1 diabetes. These infections may trigger an abnormal immune reaction in genetically at-risk children.Bacterial Infections and Chronic Inflammation
Bacteria like Helicobacter pylori may not directly mimic beta cells, but they cause long-standing inflammation. This chronic immune activation disrupts immune tolerance and increases the risk of autoimmune diseases, including Type 1 diabetes.Fungal Triggers and Immune Confusion
Fungal infections, such as those caused by Candida albicans, can also activate the immune system excessively, increasing vulnerability to autoimmune attacks in susceptible individuals.Leaky Gut and Immune Overdrive
Certain infections damage the intestinal lining, making it more permeable. This allows toxins and microbes to enter the bloodstream, creating systemic inflammation that can trigger autoimmune responses targeting the pancreas.Genetic Susceptibility Amplifies the Risk
Individuals with HLA-DR3 or HLA-DR4 gene variants are more prone to autoimmune reactions. When exposed to infections, their immune systems may be more likely to misfire against pancreatic cells.Cytokine Storms and Beta Cell Destruction
Severe infections can cause a surge in pro-inflammatory cytokines (like IL-1β and IFN-γ), which are toxic to beta cells. This environment fosters destruction even without direct viral invasion of the pancreas forcing a transplant.Vaccination Evidence Points to Protection
Interestingly, studies suggest that rotavirus vaccination may reduce the incidence of Type 1 diabetes, further hinting at a viral contribution to disease onset. This supports the theory that preventing certain infections could lower T1D risk.
In conclusion, while not every infection causes Type 1 diabetes, a combination of viral or microbial exposure, genetic predisposition, and immune dysregulation can set the stage for its development.
Viral Infections: The Suspected Culprit Behind Type 1 Diabetes
Some studies suggest that a virus causes type 1 diabetes by triggering an autoimmune response.
For example, coxsackievirus, part of the enterovirus family, has been widely studied for its potential role in diabetes development.
Furthermore, a 2019 study from the Journal of Medical Virology found a strong correlation between diabetes virus infection and the subsequent onset of Type 1 diabetes in children.
This connection is particularly concerning as it suggests that infections that many people see as routine could have long-term health consequences.
The Role of Bacterial and Fungal Infections in Type 1 Diabetes
While viral infections are often highlighted, bacterial and fungal infections should not be overlooked.
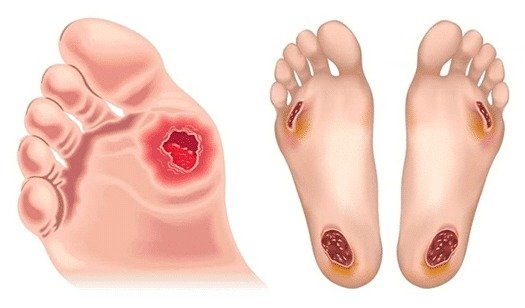
Conditions like type 1 diabetes yeast infection are common among those living with the disease.
Though these infections are usually seen as side effects, they could also be playing a more significant role.
Recent studies have shown that bacterial infections may trigger inflammatory responses that disrupt pancreatic function.
Similarly, fungal infections have been found to exacerbate autoimmune conditions. Doctors are of the opinion that airborne pollutants are also a major cause behind type 1 diabetes.
Though more research is needed, these findings suggest that bacterial and fungal infections may contribute to the worsening of autoimmune conditions like Type 1 diabetes.
Flu, Shingles, and Diabetes: What We Know So Far
Influenza and other viral illnesses are often linked to short-term blood sugar spikes, but could they also be involved in triggering Type 1 diabetes?
Research on influenza and type 1 diabetes suggests that flu infections can stress the immune system to the point where it initiates autoimmune reactions.
This makes the relationship between flu and type 1 diabetes more concerning, especially as annual flu seasons come and go.
Similarly, infections like shingles and type 1 diabetes have been associated in clinical studies.
Shingles, caused by the reactivation of the chickenpox virus, leads to inflammation that may contribute to the development or worsening of autoimmune conditions, including Type 1 diabetes.
Prevention and Management: Protecting Yourself from Infections
If infections are indeed a hidden trigger for Type 1 diabetes, what can be done to prevent this?
Vaccination and good hygiene practices can go a long way in reducing the risk of infection.
For example, getting the flu shot could not only prevent the flu but also lower the risk of triggering an autoimmune response.
Moreover, those already living with Type 1 diabetes should be particularly vigilant about preventing infections.
Since the immune system is already compromised, individuals with diabetes are more prone to complications from infections.
Strengthening the immune system through a balanced diet, regular exercise such as walking, and proper medication management can help keep infections—and diabetes-related complications—at bay.
Are Infections Really the Hidden Trigger Behind Type 1 Diabetes?
So, are infections the hidden trigger behind Type 1 diabetes?
Based on the emerging research, the answer seems to be “yes”—at least partially.
While genetics and autoimmune responses have long been understood as the primary drivers of Type 1 diabetes, infections—particularly viral infections—appear to play a significant role in triggering or accelerating the disease.
The evidence is mounting, but it is not yet conclusive.
More research is needed to fully understand the relationship between infections and Type 1 diabetes.
However, by taking steps to prevent infections and using the best dietary supplement for diabetics, we may be able to reduce the risk of developing Type 1 diabetes or minimize its complications for those already living with the condition.
References: