In this article, we will explore the relationship between gluten and Type 1 diabetes (T1D) and how gluten can influence blood sugar control.
We will examine why people with T1D are at a higher risk of celiac disease, the implications of gluten on glycemic control, and the importance of a gluten-free diet (GFD).
Scientific research and real-life examples will help us understand the hidden impact of gluten on managing diabetes.
Article Index:
- Understanding Type 1 Diabetes and Celiac Disease
- The Connection Between Gluten and Blood Sugar
- How Gluten Affects Glycemic Control in People with T1D
- The Benefits and Challenges of a Gluten-Free Diet for Blood Sugar Control
- Real-Life Example: Managing T1D and Celiac Disease
- Scientific Research on Gluten’s Impact on HbA1c Levels
- Conclusion: Is Gluten Really Affecting Blood Sugar Control?
Understanding Type 1 Diabetes and Celiac Disease
Type 1 diabetes is an autoimmune condition where the immune system mistakenly attacks insulin-producing cells in the pancreas.
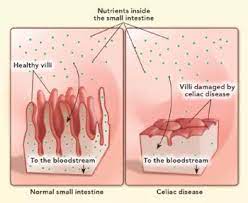
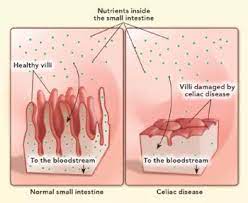
It results in lifelong dependence on insulin for blood sugar regulation. Celiac disease, another autoimmune disorder, occurs when the ingestion of gluten leads to damage in the small intestine.
Interestingly, people with T1D have a much higher likelihood of developing celiac disease compared to the general population.
Research suggests that approximately 5-10% of individuals with T1D also have celiac disease, compared to 1% in the general population.
This overlap creates challenges for managing both conditions simultaneously.
The Connection Between Gluten and Blood Sugar
For individuals juggling both Type 1 Diabetes (T1D) and celiac disease, gluten is not just a dietary nuisance—it is a metabolic landmine. The interplay between gluten and blood sugar control runs deeper than most bread crusts.
Here is a pointwise breakdown that slices through the fluff (unlike that gluten-free pancake):
Gluten and Dual Diagnosis Drama:
Gluten is a naturally occurring protein in wheat, barley, and rye. In T1D patients with co-existing celiac disease—an autoimmune gut disorder—this protein triggers immune chaos. When gluten enters the scene, the small intestine gets inflamed, which reduces its ability to absorb nutrients, including glucose-regulating ones like iron and zinc.
Malabsorption Means Mayhem:
Malnourished cells can’t do their job. According to a study in Diabetes Care, poor nutrient absorption can cause erratic blood sugar swings and unpredictable insulin needs. Think of it like trying to play darts on a moving dartboard—nearly impossible to hit your glucose target.
Inflammation: The Uninvited Guest:
Gluten exposure in celiac-positive individuals triggers intestinal inflammation, which can spill over into systemic inflammation. This impacts insulin signaling pathways, decreasing insulin sensitivity.
Translation?
More insulin needed, but less effect. A frustrating biochemical betrayal.
Going Gluten-Free = Smoother Glucose Rides:
Multiple studies, including a 2023 paper from the Journal of Pediatric Gastroenterology, show that a strict gluten-free diet helps stabilize blood sugar in T1D/celiac patients. Blood glucose levels become more predictable, insulin doses easier to fine-tune.
Real-Life Example:
Take Mia, a 14-year-old with T1D and celiac. After switching to a gluten-free diet, her HbA1c dropped from 8.2% to 7.0% in six months—and her mealtime insulin needs decreased. Coincidence? Not likely.
Bottom line: Gluten might be harmless to most, but for the T1D + celiac crowd, it is nutritional sabotage.
How Gluten Affects Glycemic Control in People with T1D
For individuals managing type 1 diabetes (T1D), controlling blood sugar levels is a delicate balance—and when celiac disease is also present, gluten becomes more than just a dietary choice.
Gluten’s role in glycemic control has been a growing area of scientific interest, particularly for those living with both T1D and celiac disease.
Improved HbA1c Levels:
Several studies have shown that people with both T1D and celiac disease who strictly follow a gluten-free diet tend to have lower HbA1c levels. This marker reflects average blood glucose over three months and is a critical indicator of long-term metabolic control.
Benefits for Children:
In children, the benefits of going gluten-free are often more pronounced. Research indicates that pediatric patients who follow a gluten-free diet shortly after their dual diagnosis experience a significant drop in HbA1c and even show improvements in cholesterol levels and body mass index.
Enhanced Insulin Sensitivity:
Some studies suggest that removing gluten from the diet may improve insulin sensitivity. Interestingly, these improvements often occur without increasing insulin dosages, implying that the body may use insulin more effectively when gluten is eliminated.
Watch the Carbs in Gluten-Free Foods:
While a gluten-free diet may benefit glycemic control, not all gluten-free foods are ideal. Many processed gluten-free products have a higher glycemic index and can cause rapid spikes in blood sugar if not carefully selected.
Potential for Long-Term Vascular Health:
Emerging research also suggests that maintaining a gluten-free diet might help reduce risks associated with diabetic microvascular complications, such as retinopathy and nephropathy, although more evidence is needed.
Tip of the Day:
For people with both T1D and celiac disease, a gluten-free diet can lead to better blood sugar control, lower HbA1c levels, and potentially fewer diabetes-related complications. However, successful management depends on a well-balanced diet, nutritional guidance, and careful carbohydrate monitoring.
The Benefits and Challenges of a Gluten-Free Diet for Blood Sugar Control
Switching to a gluten-free diet can have significant benefits for people managing both T1D and celiac disease.
By removing gluten, they reduce inflammation in the digestive tract, improving nutrient absorption and stabilizing blood sugar levels.
Additionally, a gluten-free diet may coupled with best supplements to lower blood sugar prevent spikes in blood sugar that can occur from impaired digestion.
However, a gluten-free diet comes with challenges. Gluten-free foods are often higher in carbohydrates and fats, which can affect blood sugar control.
Additionally, the social and emotional burden of adhering to a gluten-free lifestyle can be overwhelming.
Thus, managing both diabetes and celiac disease requires careful meal planning, regular blood sugar monitoring, and consistent adherence to insulin therapy.
Real-Life Example: Managing T1D and Celiac Disease
Take Lisa, a 30-year-old diagnosed with both T1D and celiac disease.
Initially, Lisa struggled with frequent blood sugar swings, even though she followed her insulin regimen.
After her celiac diagnosis, she switched to a gluten-free diet. Within months, Lisa noticed more stable blood sugar levels and her HbA1c levels improved from 8.5% to 7.2%.
This change helped her reduce the number of hypoglycemic episodes and made her overall diabetes management more predictable.
Scientific Research on Gluten’s Impact on HbA1c Levels
Scientific studies provide strong evidence that adhering to a gluten-free diet improves glycemic control in individuals with both T1D and celiac disease.
A 2019 study found that pediatric patients with both conditions who followed a strict gluten-free diet had significantly lower HbA1c levels than those who did not.
Additionally, those patients exhibited lower cholesterol levels and fewer occurrences of dyslipidemia, a common complication in diabetes.
Furthermore, research suggests that avoiding gluten may improve insulin sensitivity, potentially reducing the amount of insulin needed to maintain stable blood sugar.
While more research is needed to fully understand the mechanisms behind gluten’s impact on glycemic control, these findings highlight the importance of dietary management in diabetes care.

Is Gluten Really Affecting Blood Sugar Control?
In conclusion, gluten can indeed affect blood sugar control in people with Type 1 diabetes, especially those who also have celiac disease.
Research shows that adhering to a gluten-free diet can lead to better HbA1c levels, improved lipid profiles, and more stable blood sugar management.
For individuals managing both conditions, eliminating gluten from the diet is an essential step toward improving overall health and preventing long-term complications.
While going gluten-free may seem daunting, the benefits for people with T1D and celiac disease are clear.
Through careful dietary choices, regular monitoring, and ongoing insulin therapy, individuals can better control their blood sugar levels and enhance their quality of life.
References: