How Autoimmunity Triggers Type 1 Diabetes?
- admin
- October 5, 2024
- 8:04 am
- No Comments

Type 1 diabetes is often thought of as a condition that occurs in children and young adults when the pancreas can no longer produce insulin.
However, behind this condition lies a more complex and fascinating process—autoimmunity. This mechanism is responsible for triggering the destruction of insulin-producing cells, turning a normally functioning body into one that must rely on external insulin for survival.
But how exactly does autoimmunity lead to type 1 diabetes?
In this article, we would explore the intricate details behind this process and provide insight into why it happens.
“How Autoimmunity Triggers Type 1 Diabetes” Article Index:
- Introduction to Autoimmunity and Type 1 Diabetes
- Understanding the Immune System’s Role
- Why the Immune System Attacks the Pancreas
- The Development of Autoimmune Diabetes in Children and Adults
- Differences Between Type 1, Type 1.5, and LADA
- How Autoimmune Disorders Relate to Diabetes
- Scientific Studies on Autoimmunity and Type 1 Diabetes
- Conclusion: How Autoimmunity Triggers Type 1 Diabetes
Introduction to Autoimmunity and Type 1 Diabetes
Autoimmune diseases are conditions in which the body’s immune system mistakenly attacks its own tissues.
In the case of autoimmune diabetes, the immune system targets the beta cells in the pancreas, which are responsible for producing insulin.
When these cells are destroyed, the body can no longer produce enough insulin to regulate blood sugar levels, leading to type 1 diabetes.
But why does this happen?
Autoimmune diseases are complicated, involving a combination of genetic predisposition and environmental triggers.
In this article, we would cover in detail how autoimmunity triggers type 1 diabetes, and what sets this disease apart from other forms of diabetes.
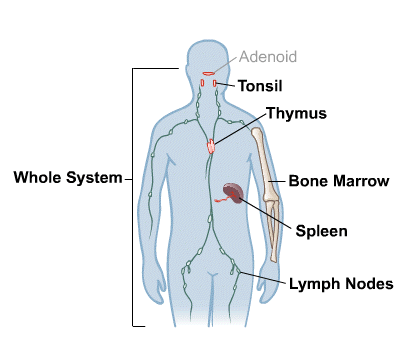
Understanding the Immune System’s Role
The immune system is like a highly trained security force designed to protect the body from harmful invaders like bacteria and viruses.
However, in autoimmune diseases, the immune system mistakenly identifies the body’s own cells as foreign and launches an attack.
In autoimmune diabetes type 1, the immune system targets and destroys the beta cells in the pancreas—the very cells that produce insulin.
Insulin is crucial for allowing glucose (sugar) to enter cells and provide them with energy.
Without enough insulin, glucose builds up in the bloodstream, leading to the high blood sugar levels associated with diabetes.
The process begins with the activation of T-cells, a type of white blood cell that normally helps fight infections.
For reasons that are still being studied, in people with type 1 diabetes, these T-cells mistakenly attack the beta cells.
Once enough beta cells are destroyed, the pancreas can no longer produce enough insulin, and diabetes develops.
So, I always suggest diabetics to include best supplements to lower blood sugar in their daily routine.
Why the Immune System Attacks the Pancreas?
So, why does the immune system suddenly turn against the pancreas?
The exact cause remains unclear, but researchers believe it involves a combination of genetics and environmental factors.
People who have certain genes are more likely to develop autoimmune disorders diabetes, including type 1 diabetes.
However, not everyone with these genes develops the condition, indicating that environmental triggers, such as viral infections or dietary factors, play a role.
There is also evidence suggesting that molecular mimicry could be involved.
This happens when the immune system confuses a viral protein with the body’s own proteins, leading to an attack on healthy cells.
In the case of type 1 diabetes, the immune system may mistakenly attack the beta cells after exposure to a virus that resembles these cells.
The Development of Autoimmune Diabetes in Children and Adults
Type 1 diabetes is most commonly diagnosed in children and young adults, but did you know that it can also develop in adults?
This form of diabetes is known as LADA latent autoimmune diabetes in adults, often referred to as type 1.5 diabetes. LADA shares characteristics with both type 1 and type 2 diabetes, but its underlying cause is still an autoimmune response.
LADA typically progresses more slowly than type 1 diabetes in children, which can make diagnosis tricky.
In fact, many adults with LADA are initially misdiagnosed with type 2 diabetes because they still produce small amounts of insulin.
However, over time, their beta cells are destroyed, and they eventually require insulin therapy, just like those with traditional type 1 diabetes.
Differences Between Type 1, Type 1.5, and LADA
Step 1: Age of Onset and Speed of Progression
Type 1 diabetes usually appears during childhood or teenage years and progresses rapidly. Individuals often experience a sudden spike in blood sugar levels, sometimes leading to diabetic ketoacidosis. In contrast, Type 1.5 diabetes—also called Latent Autoimmune Diabetes in Adults (LADA)—emerges in adulthood, typically after age 30, and progresses much more slowly. It may initially resemble type 2 diabetes due to its subtle onset.
Step 2: Autoimmunity and Immune Markers
Both Type 1 and LADA are autoimmune conditions where the immune system attacks insulin-producing beta cells. However, LADA is often associated with higher levels of certain antibodies, like GAD (glutamic acid decarboxylase), and progresses more gradually. Unlike Type 1, which causes near-total beta-cell destruction early on, LADA may retain some insulin production for years.
Step 3: Initial Treatment and Insulin Dependency
People with Type 1 require insulin therapy almost immediately after diagnosis. Those with LADA may respond to lifestyle changes or oral medications at first, but they eventually require insulin because the autoimmune attack continues. Some studies have found that starting insulin early in LADA can help preserve remaining beta-cell function.
Step 4: Misdiagnosis and Clinical Confusion
Because of its slow progression and adult onset, LADA is frequently mistaken for type 2 diabetes. Many individuals are placed on oral drugs and only receive a correct diagnosis after they fail to respond as expected. Key clues include a lean body type, lack of family history of type 2 diabetes, and poor response to oral medications.
Example:
A 40-year-old man diagnosed with type 2 diabetes failed to improve with metformin. Further tests revealed high GAD antibody levels—confirming LADA. He was switched to insulin therapy and experienced significant improvement in blood sugar control.
How Autoimmune Disorders Relate to Diabetes?
Autoimmune diseases tend to cluster, meaning that individuals with one autoimmune condition are at a higher risk of developing others.
For example, people with type 1 diabetes often have a higher likelihood of developing other autoimmune diseases such as Hashimoto’s thyroiditis, celiac disease, or vitiligo.
This clustering suggests that there may be common genetic and environmental factors that predispose individuals to multiple autoimmune conditions.
Studies have shown that the same genes that increase the risk of autoimmune diabetes type 1 also increase the risk of other autoimmune diseases.
Scientific Studies on Autoimmunity and Type 1 Diabetes
Scientific research has made significant strides in understanding the connection between autoimmunity and type 1 diabetes.
- A study published in the Journal of Autoimmunity found that genetic markers, including certain HLA genes, are strongly associated with an increased risk of developing type 1 diabetes.
- These genes help regulate the immune system, and when they are altered, they can lead to the mistaken attack on the pancreas.
- Another study from the Diabetes Journal examined how environmental triggers, such as viral infections, can lead to the development of type 1 diabetes in genetically susceptible individuals.
This study highlights the complex interplay between genetics and the environment in the development of autoimmune diabetes.
- Furthermore, research published in The Lancet has explored the potential for immunotherapy to prevent the progression of type 1 diabetes by modifying the immune response.
Although this research is still in its early stages, it offers hope that we may one day be able to intervene in the autoimmune process and prevent or delay the onset of type 1 diabetes.
How Autoimmunity Triggers Type 1 Diabetes – My Final Analysis
In conclusion, autoimmunity is at the heart of what triggers type 1 diabetes.
The immune system, designed to protect the body from harmful invaders, mistakenly attacks the insulin-producing beta cells in the pancreas.
Over time, this leads to a complete loss of insulin production, requiring people with type 1 diabetes to rely on insulin therapy for life.
The reasons why this happens are complex, involving a combination of genetic predisposition and environmental factors such as viral infections.
While researchers continue to study the exact mechanisms behind this autoimmune attack, it is clear that once the immune system begins destroying beta cells, the progression toward diabetes is inevitable.
While there is no cure for type 1 diabetes, understanding its autoimmune origins helps us appreciate the complexity of the condition and why it develops.
This knowledge can also guide future research into treatments that may one day stop the autoimmune attack and preserve beta-cell function, potentially preventing the development of type 1 diabetes in those at risk.
References: