How Chromosomal Abnormalities Trigger Neonatal Diabetes?
- admin
- December 14, 2024
- 4:59 pm
- No Comments
Neonatal diabetes is a rare form of diabetes that typically occurs in infants and is often associated with genetic factors, specifically chromosomal abnormalities.
This condition can manifest in the first six months of life and often leads to challenges in managing blood glucose levels.
While neonatal diabetes can arise due to mutations in specific genes, chromosomal abnormalities also play a significant role in triggering this form of diabetes.
This article by bestdietarysupplementfordiabetics.com delves into how chromosomal abnormalities lead to neonatal diabetes, the underlying mechanisms, and provides real-life examples of how this condition affects individuals.
Article Index:
- Introduction to Neonatal Diabetes and Chromosomal Abnormalities
- Understanding Chromosomal Abnormalities and Their Role in Neonatal Diabetes
- 2.1. Genetic and Chromosomal Factors in Diabetes
- 2.2. Specific Chromosomal Abnormalities Linked to Neonatal Diabetes
- Mechanisms of Diabetes Triggered by Chromosomal Abnormalities
- 3.1. Impaired Insulin Secretion Due to Genetic Mutations
- 3.2. The Role of Chromosomal Aberrations in Beta-Cell Dysfunction
- Real-Life Examples of Chromosomal Abnormalities Leading to Neonatal Diabetes
- 4.1. Case Study: A Baby with 6q24-Related Neonatal Diabetes
- 4.2. Case Study: Neonatal Diabetes Caused by 11p13 Chromosomal Deletion
- The Link Between Chromosomal Abnormalities and Endocrine Disruptions
- Scientific Studies and Findings on Chromosomal Abnormalities and Neonatal Diabetes
- FAQs on Neonatal Diabetes and Chromosomal Abnormalities
- Conclusion: Understanding Chromosomal Abnormalities as a Cause of Neonatal Diabetes
Introduction to Neonatal Diabetes and Chromosomal Abnormalities
Neonatal diabetes is a rare and genetically driven condition that typically appears in infants under the age of six months.
Unlike the more common forms of diabetes such as Type 1 and Type 2 diabetes, neonatal diabetes often results from specific genetic mutations or chromosomal abnormalities that disrupt normal insulin production in the pancreas.
The condition is often permanent, requiring lifelong management. While some mutations in individual genes contribute to neonatal diabetes, chromosomal abnormalities, which involve larger structural changes in chromosomes, can also play a crucial role in its development.
These abnormalities can lead to dysfunction in the pancreas, specifically in the beta cells that produce insulin, thereby impairing glucose regulation.
In this article, we explore how chromosomal abnormalities are linked to neonatal diabetes, the mechanisms by which they trigger the condition, and provide real-life case studies to understand the impact of these genetic changes.
Understanding Chromosomal Abnormalities and Their Role in Neonatal Diabetes
Let us walk you through these in brief:
Genetic and Chromosomal Factors in Diabetes:
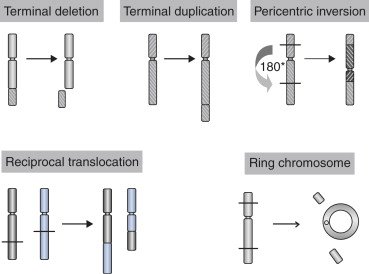
Chromosomal abnormalities refer to changes in the structure or number of chromosomes that can lead to developmental or functional disruptions in various organs, including the pancreas.
In the case of neonatal diabetes, these abnormalities can cause beta-cell dysfunction, reduced insulin production, and poor glucose regulation.
Diabetes caused by chromosomal abnormalities is typically diagnosed in infancy, and it often presents as hyperglycemia (high blood sugar).
The mutations or structural changes in the chromosomes can be inherited or occur spontaneously, affecting one or more genes involved in insulin production, processing, and secretion.
Specific Chromosomal Abnormalities Linked to Neonatal Diabetes:
Several chromosomal abnormalities are known to contribute to neonatal diabetes.
For example, changes in chromosome 6, 11, and 12 have been associated with neonatal diabetes, each causing disruptions in different genetic regions responsible for insulin production.
- 6q24-related Neonatal Diabetes: This chromosomal abnormality is one of the most common genetic causes of neonatal diabetes. It is characterized by duplications or deletions of a region on chromosome 6, which leads to abnormal insulin production.
- 11p13 Deletions: This is another chromosomal abnormality that has been linked to neonatal diabetes. It affects genes that regulate the development and function of pancreatic beta cells.
Mechanisms of Diabetes Triggered by Chromosomal Abnormalities
A quick look at these in brief:
Impaired Insulin Secretion Due to Genetic Mutations:
One of the primary mechanisms by which chromosomal abnormalities lead to neonatal diabetes is through impaired insulin secretion.
In a typical individual, the pancreas produces insulin, which helps regulate blood glucose levels. However, chromosomal abnormalities can result in defective insulin production or processing.
For instance, a mutation in chromosome 6q24 can lead to the overexpression of certain genes that inhibit normal insulin production in beta cells.
As a result, the pancreas fails to secrete adequate amounts of insulin, leading to sustained high blood sugar levels.
Similarly, chromosomal deletions or duplications can interfere with the normal genetic pathways responsible for insulin secretion, leading to a state of insulin deficiency.
The Role of Chromosomal Aberrations in Beta-Cell Dysfunction:
Chromosomal abnormalities can also impact the development and function of beta cells, which are responsible for producing insulin in the pancreas.
For example, chromosomal rearrangements in the 11p13 region have been shown to disrupt the normal functioning of pancreatic beta cells.
These disruptions can lead to beta-cell dysfunction, making it difficult for the pancreas to produce sufficient insulin to maintain normal blood sugar levels.
Additionally, chromosomal abnormalities can affect the genetic instructions necessary for the differentiation of beta cells in the developing pancreas.
This results in fewer beta cells, further exacerbating insulin deficiency.
As a result, neonatal diabetes develops as the body struggles to manage glucose levels without adequate insulin production.
Real-Life Examples of Chromosomal Abnormalities Leading to Neonatal Diabetes
Here are 2 classic cases that we would like to discuss:
A Baby with 6q24-Related Neonatal Diabetes:
A three-month-old infant, Emma, was diagnosed with neonatal diabetes after presenting with persistent high blood glucose levels.
Genetic testing revealed a duplication on chromosome 6, specifically in the 6q24 region, which led to the overproduction of certain proteins that inhibited insulin secretion.
As a result, Emma’s pancreas was unable to produce sufficient insulin to regulate her blood glucose levels.
The family history of diabetes further suggested a genetic predisposition, and Emma’s case was confirmed as 6q24-related neonatal diabetes.
Early diagnosis allowed for a shift from insulin injections to oral medication, improving insulin secretion and stabilizing her glucose levels.
This case highlights the critical role of genetic testing in identifying chromosomal abnormalities as a cause of neonatal diabetes.
Neonatal Diabetes Caused by 11p13 Chromosomal Deletion:
A second case involved a newborn, Alex, who was diagnosed with neonatal diabetes due to a deletion on chromosome 11p13.
This chromosomal abnormality led to beta-cell dysfunction and insufficient insulin production. Alex’s condition was diagnosed through genetic screening after doctors observed persistent hyperglycemia and failure to thrive.
Unlike Emma’s case, Alex’s condition required lifelong insulin therapy, as his pancreas could not produce enough insulin to regulate his blood sugar.
Genetic counseling revealed that Alex’s parents carried a recessive copy of the 11p13 deletion, which was passed down to their child.
Early intervention helped manage Alex’s condition, but the genetic cause of his neonatal diabetes remained a lifelong challenge.
The Link Between Chromosomal Abnormalities and Endocrine Disruptions
Chromosomal abnormalities can cause a variety of endocrine disruptions, especially in the pancreas, leading to neonatal diabetes.
The pancreas is responsible for the production of both insulin and glucagon, hormones that regulate blood sugar levels.
Disruptions in the genetic pathways that govern insulin production can lead to a deficiency in this hormone, which results in the inability to maintain normal glucose levels.
In addition to insulin, chromosomal abnormalities can also affect other aspects of pancreatic function, such as glucagon regulation and beta-cell differentiation.
These disruptions further contribute to the development of neonatal diabetes and make it difficult for affected individuals to regulate their blood glucose levels effectively.
Scientific Studies and Findings on Chromosomal Abnormalities and Neonatal Diabetes
Several studies have examined the connection between chromosomal abnormalities and neonatal diabetes, revealing insights into the underlying mechanisms that trigger the condition.
- Diabetologia Study (Støy et al., 2007): This study identified the 6q24 duplication as a significant cause of neonatal diabetes and emphasized the importance of genetic testing for early diagnosis and intervention.
- Nature Genetics Study (Bellanné-Chantelot et al., 2009): Researchers highlighted the role of 11p13 chromosomal deletions in neonatal diabetes and linked this abnormality to beta-cell dysfunction and insulin resistance.
- Human Molecular Genetics (Kawakami et al., 2011): This study focused on the genetic pathways involved in neonatal diabetes, particularly how chromosomal abnormalities lead to impaired insulin production and glucose metabolism.
These studies, among others, provide critical insight into the role of chromosomal abnormalities in the development of neonatal diabetes and underscore the importance of early genetic diagnosis.
FAQs on Neonatal Diabetes and Chromosomal Abnormalities
Q-1: Which chromosomal changes most commonly trigger neonatal diabetes—and how?
A-1: The best-known hotspot is 6q24. When paternally active genes there (notably PLAGL1 and HYMAI) are overexpressed—because of a paternal 6q24 duplication, paternal uniparental disomy of chromosome 6, or loss of maternal methylation—newborns produce too little insulin. This typically causes transient neonatal diabetes in the first weeks of life.
Q-2: Can errors in imprinting machinery present like a chromosomal neonatal diabetes case?
A-2: Yes. Mutations in imprinting regulators such as ZFP57 can create multilocus imprinting disturbances, including hypomethylation at 6q24. Although ZFP57 is a single-gene issue, the downstream effect mimics a chromosome-level imprinting error, so methylation testing is crucial alongside copy-number analysis when 6q24-related transient neonatal diabetes is suspected.
Q-3: Which chromosomal microdeletions impair pancreas development and lead to early insulin failure?
A-3: Deletions involving GATA6 (often at 18q11.2) can cause pancreatic agenesis or hypoplasia with neonatal diabetes, frequently accompanied by congenital heart or hepatobiliary anomalies. Deletions at 17q12 that include HNF1B may produce diabetes with pancreatic structural changes plus renal cysts. Recognizing these copy-number syndromes guides both genetic work-up and organ-system surveillance.
Q-4: What clinical clues suggest a chromosomal cause rather than a KATP-channel mutation?
A-4: Think chromosomal when there is severe intrauterine growth restriction with hyperglycaemia in week one (classic for 6q24-related disease), multisystem or dysmorphic features (e.g., heart defects with GATA6; renal cysts/pancreatic dysplasia with HNF1B deletions), and a weak response to high-dose sulfonylureas (which often help KATP-channel cases). Family history may be negative because duplications or methylation errors are frequently de novo.
Q-5: What testing pathway best captures chromosomal and imprinting lesions in neonatal diabetes?
A-5: If transient neonatal diabetes is suspected, begin with 6q24 methylation analysis and testing for paternal uniparental disomy of chromosome 6. Add copy-number assays (chromosomal microarray or MLPA) to detect paternal 6q24 duplications and broader CNVs such as GATA6 (18q11.2) or HNF1B (17q12). When 6q24 hypomethylation is found, evaluate for ZFP57 variants indicating a multilocus imprinting disturbance. Early, precise diagnosis informs therapy, relapse monitoring in 6q24 disease, and targeted screening for associated organ anomalies.
Conclusion: Understanding Chromosomal Abnormalities as a Cause of Neonatal Diabetes
Chromosomal abnormalities are a significant cause of neonatal diabetes, a rare but serious condition that often presents in the first few months of life.
Disruptions in the genes responsible for pancreatic function, particularly those related to insulin production, lead to the development of this form of diabetes.
Early diagnosis through genetic testing is crucial, as it enables proper management and tailored interventions to regulate glucose levels.
Real-life case studies, such as those involving 6q24 duplications and 11p13 deletions, provide valuable insight into how these chromosomal abnormalities contribute to neonatal diabetes.
While the condition remains challenging to manage, understanding the genetic basis of neonatal diabetes is crucial for improving outcomes and providing personalized care.
Genetic counseling and early interventions, including insulin therapy and medication, can help individuals with neonatal diabetes lead healthy lives.
Further research into chromosomal abnormalities and their role in neonatal diabetes will continue to shed light on potential treatment strategies and enhance our understanding of this complex condition.
References: