How Dominant Mutations in the KCNJ11 Gene Lead to Neonatal Diabetes?
- admin
- December 24, 2024
- 7:32 pm
- No Comments
Neonatal diabetes is a rare form of diabetes that manifests in the first six months of life, affecting approximately 1 in 100,000 to 500,000 live births.
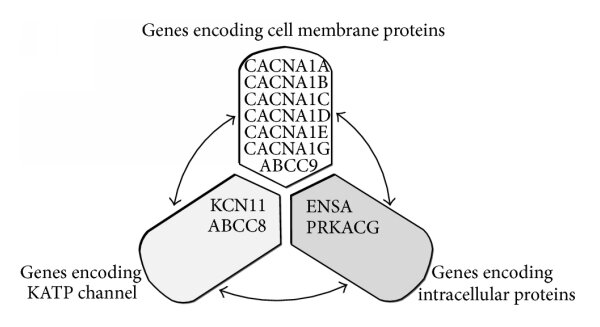
One of the leading genetic causes of neonatal diabetes is mutations in the KCNJ11 gene. This gene encodes the Kir6.2 protein, a critical component of the ATP-sensitive potassium (KATP) channel in pancreatic beta cells.
Dominant mutations in KCNJ11 disrupt the function of this channel, impairing insulin secretion and leading to hyperglycemia.
In this article, we will explore the biological mechanisms linking KCNJ11 mutations to neonatal diabetes, the types of mutations involved, their physiological consequences, and real-life examples.
We will also examine the scientific research that illuminates this connection.
Article Index:
- Understanding the KCNJ11 Gene and the KATP Channel
- Mechanisms of Insulin Secretion and the Role of KCNJ11
- Dominant Mutations in KCNJ11: Types and Effects
- How KCNJ11 Mutations Disrupt Beta Cell Function
- Physiological Consequences of KCNJ11 Mutations
- Scientific Evidence Linking KCNJ11 Mutations to Neonatal Diabetes
- Real-Life Examples: Clinical Presentations
- Conclusion: The Impact of KCNJ11 Mutations on Neonatal Diabetes
Understanding the KCNJ11 Gene and the KATP Channel
The KCNJ11 gene, located on chromosome 11, is vital for glucose metabolism. It encodes the Kir6.2 subunit of the ATP-sensitive potassium (KATP) channel found in pancreatic beta cells.
This channel plays a critical role in regulating insulin secretion, a process essential for maintaining normal blood glucose levels.
The KATP channel is composed of two primary subunits: Kir6.2, which forms the potassium ion pore, and SUR1 (encoded by the ABCC8 gene), which modulates the channel’s activity and response to cellular changes.
How the KATP Channel Functions:
Under normal conditions, the KATP channel acts as a metabolic sensor in beta cells. When blood glucose levels rise, glucose metabolism in the beta cells increases the ATP/ADP ratio. This elevated ratio causes the KATP channels to close, leading to membrane depolarization.
Triggering Insulin Secretion:
Membrane depolarization activates voltage-gated calcium channels, allowing calcium ions to enter the beta cells. This calcium influx is a critical signal that triggers the exocytosis of insulin granules, releasing insulin into the bloodstream. This process ensures the regulation of blood glucose levels and relies on the proper functioning of the KCNJ11 gene.
Impact of Mutations in KCNJ11:
The structural and functional integrity of the KCNJ11 gene is essential for the effective operation of the KATP channel. Mutations or disruptions in this gene impair insulin secretion and can lead to serious conditions such as neonatal diabetes.
Mechanisms of Insulin Secretion and the Role of KCNJ11
Insulin secretion is a tightly regulated process essential for maintaining blood glucose homeostasis, and the KATP channel is central to this regulation.
This channel acts as a sensor, linking cellular energy levels to insulin release.
Under normal conditions, the KATP channel remains open in low-glucose states, allowing potassium ions to exit the cell and maintaining the cell’s resting membrane potential.
When glucose levels rise, glucose metabolism increases the intracellular ATP/ADP ratio. The elevated ATP binds to the Kir6.2 subunit of the KATP channel, causing it to close.
This closure depolarizes the cell membrane, which activates voltage-dependent calcium channels.
Calcium ions then enter the beta cell, triggering the fusion of insulin vesicles with the plasma membrane and the release of insulin into the bloodstream.
Mutations in the KCNJ11 gene disrupt this finely tuned process by impairing the channel’s ability to respond to ATP, leading to impaired insulin secretion and hyperglycemia, which are hallmarks of neonatal diabetes.
Dominant Mutations in KCNJ11: Types and Effects
Dominant mutations in the KCNJ11 gene often result in a gain-of-function effect, where the ATP-sensitive potassium (KATP) channel becomes less responsive to ATP.
This defect prevents the channel from closing properly, even in the presence of high glucose levels, disrupting the insulin secretion process.
Normally, the closure of the KATP channel is essential for membrane depolarization, a critical step required to trigger insulin release.
However, when the channel remains persistently open due to mutations, it hinders this pathway, leading to hyperglycemia and the onset of neonatal diabetes.
E23K Mutation:
One such mutation is E23K, where glutamic acid is replaced by lysine at position 23. This change increases the activity of the channel, reducing its responsiveness to ATP and impairing normal glucose-stimulated insulin release.
R201H and R201C Mutations:
Another set of common mutations, R201H and R201C, are strongly associated with neonatal diabetes. These mutations significantly impair the channel’s ability to regulate its open and closed states, resulting in reduced insulin secretion and chronic hyperglycemia.
V59M Mutation and Severe Effects:
The V59M mutation leads to more severe conditions, such as developmental delay, epilepsy, and neonatal diabetes (DEND syndrome). This mutation highlights the broader impact of KCNJ11 mutations, affecting both glucose regulation and neurological development.
Summary of Mutation Effects
These mutations cause the KATP channel to remain in an open state, significantly diminishing the beta cells’ capacity to depolarize and secrete insulin in response to glucose. This dysfunction underscores the critical role of the KCNJ11 gene in maintaining proper insulin secretion and blood glucose homeostasis.
How KCNJ11 Mutations Disrupt Beta Cell Function?
Mutations in the KCNJ11 gene lead to persistent activity of the ATP-sensitive potassium (KATP) channel, preventing the crucial process of membrane depolarization in pancreatic beta cells.
This disruption has several downstream consequences that impair insulin secretion and contribute to the pathophysiology of neonatal diabetes.
Reduced Calcium Influx:
Membrane depolarization is essential for activating voltage-dependent calcium channels.
When the KATP channel remains open, these calcium channels stay closed, significantly reducing calcium entry into the beta cells.
Without sufficient intracellular calcium, the signaling required for insulin release is disrupted.
Impaired Insulin Exocytosis:
Calcium plays a vital role in triggering the fusion of insulin granules with the cell membrane.
Reduced calcium influx leads to a significant decrease in insulin secretion, contributing to chronic hyperglycemia.
Beta Cell Exhaustion:
Persistent hyperglycemia caused by inadequate insulin secretion places excessive stress on beta cells, leading to their overwork and eventual dysfunction or apoptosis.
Over time, this further exacerbates the insulin deficiency.
These effects highlight the critical role of KCNJ11 mutations in neonatal diabetes, demonstrating how even small disruptions in cellular mechanisms can lead to significant metabolic consequences.
Physiological Consequences of KCNJ11 Mutations
The physiological consequences of KCNJ11 mutations manifest primarily as neonatal diabetes, but the severity and associated symptoms can vary depending on the specific mutation.
Isolated Neonatal Diabetes:
- Characterized by hyperglycemia diagnosed within the first six months of life.
- Requires insulin or sulfonylurea therapy to manage blood glucose levels.
DEND Syndrome:
- Severe mutations like V59M can lead to developmental delay, epilepsy, and neonatal diabetes.
- Neurological symptoms result from KATP channel dysfunction in the brain, where Kir6.2 also plays a role.
Example: A study published in The New England Journal of Medicine (2006) by Gloyn et al. identified over 20 KCNJ11 mutations associated with neonatal diabetes.
Among these, patients with R201H mutations showed isolated diabetes, while those with V59M mutations exhibited more severe systemic effects.
Scientific Evidence Linking KCNJ11 Mutations to Neonatal Diabetes
Several studies have established the link between KCNJ11 mutations and neonatal diabetes:
- Gloyn et al., 2004: This groundbreaking study in The New England Journal of Medicine identified KCNJ11 mutations as a cause of permanent neonatal diabetes, explaining the genetic basis of the disease.
- Proks et al., 2006: Published in Diabetes, this study demonstrated how specific KCNJ11 mutations alter KATP channel activity, leading to impaired insulin secretion.
- Slingerland et al., 2006: This research in Diabetologia emphasized the spectrum of phenotypes associated with KCNJ11 mutations, ranging from isolated diabetes to syndromic presentations like DEND.
These studies provide a robust framework for understanding the molecular mechanisms of neonatal diabetes.
Clinical Presentations
Isolated Neonatal Diabetes Maria, a 3-month-old infant, was diagnosed with persistent hyperglycemia after failing to gain weight and experiencing dehydration. Genetic testing revealed an R201H mutation in KCNJ11. Maria’s condition was managed effectively with sulfonylurea therapy, which enhanced insulin secretion by closing the mutated KATP channels.
Neonatal Diabetes with Neurological Symptoms James, a 6-month-old boy, presented with hyperglycemia, developmental delays, and seizures. Genetic analysis identified the V59M mutation in KCNJ11, confirming DEND syndrome. His treatment required both sulfonylureas and targeted therapies for his neurological symptoms.
Transition from Insulin to Sulfonylureas Emma, diagnosed with neonatal diabetes at 2 months, initially required insulin therapy. Genetic testing later revealed an E23K mutation in KCNJ11. She successfully transitioned to sulfonylureas, which improved her glycemic control and quality of life.
The Impact of KCNJ11 Mutations on Neonatal Diabetes
Dominant mutations in the KCNJ11 gene impair the ATP-sensitive potassium (KATP) channel in pancreatic beta cells, disrupting insulin secretion and leading to neonatal diabetes.
These mutations result in a spectrum of symptoms, ranging from isolated hyperglycemia to severe conditions like developmental delay, epilepsy, and neonatal diabetes (DEND syndrome).
Research, including studies in The New England Journal of Medicine (2006), has identified over 20 mutations linked to this condition.
Advances in understanding the molecular mechanisms have revolutionized treatment, with targeted therapies like sulfonylureas restoring insulin secretion in many cases.
Ongoing research aims to refine diagnostic tools and optimize outcomes for affected patients.
References: