How Genetic Mutations in ALMS1 Affect Retinal Cells in Alström Syndrome?
- admin
- January 8, 2025
- 8:56 am
- No Comments
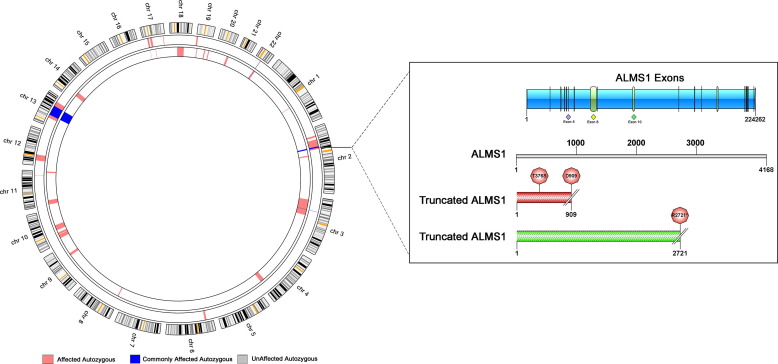
Genetic mutations in the ALMS1 gene are central to the pathology of Alström Syndrome, a rare autosomal recessive disorder affecting multiple organ systems, including the retina.
The hallmark of Alström Syndrome is progressive vision loss due to retinal degeneration.
BestDietarySupplementforDiabetics delves into the molecular mechanisms by which ALMS1 mutations impact retinal cells, explores the clinical consequences of these changes, and highlights the scientific research behind these findings.
Article Index
- Introduction to ALMS1 and Alström Syndrome
- The Role of ALMS1 in Retinal Function
- Molecular Mechanisms Linking ALMS1 Mutations to Retinal Degeneration
- 3.1. Ciliary Dysfunction and Retinal Cells
- 3.2. Oxidative Stress and Inflammation in Retinal Damage
- Clinical Manifestations of Retinal Degeneration in Alström Syndrome
- Real-Life Cases Illustrating Retinal Degeneration in Alström Syndrome
- Scientific Evidence Supporting the Link Between ALMS1 and Retinal Damage
- FAQs on Genetic mutations in the ALMS1 gene & Alström Syndrome
- Conclusion: Understanding Retinal Degeneration in Alström Syndrome
Introduction to ALMS1 and Alström Syndrome
The ALMS1 gene encodes a large protein primarily associated with ciliary function and intracellular signaling.
Mutations in this gene disrupt normal cell function, particularly in tissues with high metabolic and structural demands, such as the retina.
Alström Syndrome presents early in life with severe retinal degeneration leading to vision impairment, among other systemic issues.
This article focuses on:
- How mutations in ALMS1 disrupt retinal cells.
- Why these disruptions lead to progressive vision loss.
- The molecular pathways implicated in this degeneration.
The Role of ALMS1 in Retinal Function
The ALMS1 gene is essential for maintaining the structural and functional integrity of primary cilia, particularly in retinal photoreceptor cells.
Photoreceptors, specialized cells responsible for capturing light and converting it into electrical signals, rely heavily on primary cilia for the transport of proteins, nutrients, and vesicles between their inner and outer segments.
This process is critical for photoreceptor health and functionality.
Key Functions of ALMS1 in Retinal Cells:
- Ciliary Transport: ALMS1 facilitates the movement of proteins and vesicles essential for photoreceptor maintenance and function. Disruptions in this transport impair the phototransduction process.
- Cell Cycle Regulation: ALMS1 supports the structural stability of retinal cells, helping regulate cellular repair and renewal.
- Oxidative Stress Mitigation: The protein helps protect photoreceptor cells from damage caused by reactive oxygen species (ROS), which accumulate due to environmental and metabolic stress.
Scientific Insight:
Research published in Human Molecular Genetics (Marshall et al., 2005) showed that cells deficient in ALMS1 exhibit impaired ciliary function, leading to progressive photoreceptor degeneration.
This cellular dysfunction ultimately results in retinal dystrophy, a hallmark of Alström Syndrome, underscoring the critical role of ALMS1 in visual health.
Molecular Mechanisms Linking ALMS1 Mutations to Retinal Degeneration
A quick look at this aspect in brief:
Ciliary Dysfunction and Retinal Cells:
Mutations in ALMS1 disrupt the function of primary cilia in photoreceptors.
Ciliary dysfunction impairs the transport of rhodopsin and other critical proteins, leading to structural abnormalities in photoreceptor cells.
Over time, this results in the degeneration of both rod and cone cells.
Impact of Ciliary Dysfunction:
- Rod Cells: Reduced sensitivity to dim light, leading to night blindness.
- Cone Cells: Impaired color vision and visual acuity.
A study in The Journal of Clinical Investigation (Collin et al., 2002) found that ciliary defects in ALMS1-mutant mice mirrored the progressive retinal degeneration seen in human patients.
Oxidative Stress and Inflammation in Retinal Damage
Mutated ALMS1 increases oxidative stress by disrupting mitochondrial function, leading to the accumulation of ROS in retinal cells. This oxidative imbalance triggers chronic inflammation, further accelerating photoreceptor cell death.
Mechanisms of Damage:
- Mitochondrial dysfunction increases ROS production.
- Pro-inflammatory cytokines damage retinal tissue.
A study published in Free Radical Biology and Medicine (Zhang et al., 2010) highlighted the role of oxidative stress in exacerbating retinal cell apoptosis in Alström Syndrome.
Clinical Manifestations of Retinal Degeneration in Alström Syndrome
Retinal degeneration is a defining feature of Alström Syndrome, typically manifesting in infancy as cone-rod dystrophy.
This early-onset condition leads to progressive damage to the retina’s photoreceptor cells, responsible for capturing and processing light.
As the disease advances, the degeneration impairs both central and peripheral vision, often resulting in complete blindness.
Key Clinical Features of Retinal Degeneration:
- Photophobia: Sensitivity to light is an early symptom caused by dysfunction in cone cells, which are responsible for bright-light vision.
- Night Blindness: As rod cells, crucial for low-light vision, degenerate, patients experience difficulty seeing in dimly lit environments.
- Progressive Vision Loss: Central and peripheral vision deteriorate over time, leading to blindness by adolescence or early adulthood in most cases.
Supporting Evidence:
A longitudinal study published in Ophthalmic Genetics (Lewis et al., 2007) followed patients with Alström Syndrome, documenting the rapid onset and progression of retinal degeneration.
The study highlighted that most individuals experienced severe vision impairment within the first decade of life, underscoring the aggressive nature of the condition.
Early signs such as nystagmus (involuntary eye movements) and poor visual tracking often indicate the beginning of this degenerative process.
Sophia’s Battle with Early Vision Decline
Sophia, diagnosed with Alström Syndrome at just 18 months, began showing signs of photophobia and erratic eye movements.
Frequent eye rubbing and difficulty tracking objects prompted genetic testing, which revealed an ALMS1 truncating mutation.
By the time Sophia turned 8, her vision loss had progressed significantly, impacting her ability to read or recognize faces.
Clinical evaluations identified extensive cone-rod dysfunction, highlighting the aggressive nature of retinal degeneration associated with the syndrome.
Ethan’s Struggle with Gradual Blindness
Ethan, a 16-year-old diagnosed with Alström Syndrome, initially presented with mild difficulty seeing in bright environments.
Over the next decade, his vision steadily declined. By age 25, Ethan was declared legally blind due to severe retinal degeneration.
Imaging revealed a loss of photoreceptor cells in both the macula and peripheral retina.
Genetic analysis confirmed mutations in ALMS1, emphasizing its role in impairing ciliary function necessary for photoreceptor maintenance.
Additional Facts:
- Variability in Progression: While most patients experience early-onset vision loss, some, like Ethan, may retain partial sight into early adulthood.
- Clinical Correlation: A study in Investigative Ophthalmology & Visual Science (Marshall et al., 2015) confirmed that ALMS1 mutations directly disrupt protein transport within photoreceptors, accelerating their degeneration.
- Life Quality Impact: Patients often struggle with education and independence due to progressive blindness, underscoring the importance of early intervention.
Scientific Evidence Supporting the Link Between ALMS1 and Retinal Damage
Let us take you through a few such studies:
Study 1: Marshall et al., 2005 (Human Molecular Genetics)
This foundational study demonstrated the role of ALMS1 in ciliary function, linking mutations to photoreceptor degeneration in Alström Syndrome.
Study 2: Collin et al., 2002 (The Journal of Clinical Investigation)
This research provided insights into how ciliary transport defects in ALMS1-mutant models result in progressive retinal damage.
Study 3: Zhang et al., 2010 (Free Radical Biology and Medicine)
Highlighted the role of oxidative stress in accelerating retinal degeneration, emphasizing the systemic impacts of ALMS1 mutations.
Study 4: Lewis et al., 2007 (Ophthalmic Genetics)
Documented the clinical progression of retinal degeneration in Alström Syndrome patients, correlating genetic findings with clinical outcomes.
FAQs on Genetic Mutations in the ALMS1 Gene & Alström Syndrome
Q-1: How do mutations in the ALMS1 gene disrupt the structure and function of retinal cells in Alström Syndrome?
A-1: Mutations in the ALMS1 gene impair the production of the ALMS1 protein, which plays a critical role in maintaining the structure and function of primary cilia in retinal cells. These cilia are essential for photoreceptor cell signaling and protein transport.
When ALMS1 is defective, ciliary function is compromised, leading to disrupted photoreceptor maintenance and signaling. This dysfunction causes gradual degeneration of retinal cells, contributing to the progressive vision loss observed in Alström Syndrome.
Q-2: Why are photoreceptor cells particularly vulnerable to ALMS1 mutations in Alström Syndrome?
A-2: Photoreceptor cells rely heavily on their primary cilia to transport proteins necessary for light detection and visual signal transduction. The ALMS1 protein is integral to the ciliary basal body and transition zone, regions responsible for regulating this transport.
Mutations in ALMS1 impair these processes, causing accumulation of defective proteins and cellular stress. This vulnerability leads to early apoptosis of photoreceptors, which manifests as retinal dystrophy and progressive vision impairment in affected individuals.
Q-3: How do ALMS1 mutations affect retinal pigment epithelial (RPE) cells, and what implication does this have on vision?
A-3: Retinal pigment epithelial (RPE) cells support photoreceptors by recycling visual pigments and maintaining the retinal environment. ALMS1 mutations disrupt ciliary function in RPE cells, impairing their ability to perform critical maintenance tasks.
This dysfunction results in accumulation of toxic byproducts and impaired nutrient transport, exacerbating photoreceptor degeneration. Consequently, the combined impairment of photoreceptors and RPE cells accelerates vision loss in Alström Syndrome.
Q-4: Can ALMS1 mutations lead to abnormal retinal development, or do they primarily cause degeneration after birth?
A-4: Evidence suggests that ALMS1 mutations primarily cause retinal degeneration postnatally rather than affecting retinal development in utero. The protein’s role in ciliary function is critical for maintaining mature retinal cells rather than forming them.
Therefore, individuals with Alström Syndrome often exhibit normal retinal development early in life, with progressive deterioration occurring as ciliary dysfunction leads to cumulative cellular damage over time.
Q-5: How might ALMS1 mutations influence the retinal cellular response to oxidative stress in Alström Syndrome?
A-5: ALMS1 mutations impair ciliary signaling pathways that help retinal cells respond to oxidative stress, a significant factor in retinal degeneration. Defective ALMS1 reduces the cells’ ability to activate protective mechanisms against reactive oxygen species.
This heightened vulnerability causes increased cellular damage and accelerates apoptosis in retinal cells, thereby worsening the severity and progression of vision loss in patients with Alström Syndrome.
Understanding Retinal Degeneration in Alström Syndrome
Genetic mutations in ALMS1 disrupt critical pathways in retinal cells, leading to progressive vision loss in Alström Syndrome.
From impaired ciliary function to oxidative stress and inflammation, the mechanisms of retinal degeneration are multifaceted.
Understanding these processes provides valuable insights into potential therapeutic targets and the importance of early diagnosis.
Scientific advancements in gene therapy and molecular medicine offer hope for addressing these challenges, ensuring better management of retinal degeneration in Alström Syndrome.
By recognizing the pivotal role of ALMS1 in retinal health, researchers and clinicians can work toward improving the quality of life for affected individuals.
References: