How Genetic Mutations in INS Cause Neonatal Diabetes?
- admin
- December 11, 2024
- 7:33 pm
- No Comments
Neonatal diabetes mellitus (NDM) is a rare form of diabetes that manifests within the first six months of life.
Unlike other types of diabetes, which are typically influenced by lifestyle or autoimmune factors, NDM is often caused by genetic mutations that impair insulin production.
One of the most critical genes involved in this condition is INS, which encodes insulin, a hormone essential for regulating blood glucose levels.
Mutations in the INS gene disrupt insulin synthesis, folding, or secretion, leading to severe hyperglycemia in affected infants.
BestDietarySupplementforDiabetics delves into the mechanisms by which INS mutations cause neonatal diabetes, explores scientific research on the topic, and highlights real-life cases to provide a comprehensive understanding.
Table of Contents
- Introduction to Neonatal Diabetes and the INS Gene
- Mechanisms of INS Mutations Leading to Neonatal Diabetes
- 2.1. Impaired Insulin Production
- 2.2. Protein Misfolding and ER Stress
- 2.3. Disrupted Insulin Secretion Pathways
- Types of INS Gene Mutations and Their Impact
- 3.1. Missense Mutations
- 3.2. Frameshift Mutations
- 3.3. Dominant-Negative Mutations
- Real-Life Cases of INS Mutations in Neonatal Diabetes
- 4.1. Case Study: Genetic Diagnosis in a Newborn
- 4.2. Case Study: Familial INS Mutations
- FAQs on Genetic Mutations in INA Genes & Neonatal Diabetes
- Conclusion
Introduction to Neonatal Diabetes and the INS Gene
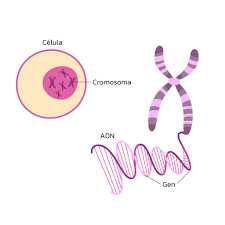
The INS gene, located on chromosome 11, encodes proinsulin, a precursor that undergoes processing to form functional insulin.
This hormone, produced by the beta cells of the pancreas, is essential for maintaining glucose homeostasis by facilitating glucose uptake into cells.
Mutations in the INS gene disrupt the synthesis, processing, or secretion of insulin, leading to neonatal diabetes mellitus (NDM)—a rare condition that manifests within the first six months of life.
NDM is divided into transient neonatal diabetes mellitus (TNDM), which resolves within months, and permanent neonatal diabetes mellitus (PNDM), which requires lifelong management.
INS mutations are most commonly linked to PNDM, where disrupted insulin production results in persistent hyperglycemia.
A pivotal study published in Diabetologia (Støy et al., 2007) identified INS mutations as a leading cause of PNDM, highlighting the gene’s critical role in early glucose regulation.
These findings underscore the importance of genetic screening for accurate diagnosis and management of neonatal diabetes, providing targeted therapeutic options for affected infants.
Mechanisms of INS Mutations Leading to Neonatal Diabetes
Here is how it works in real life;
Impaired Insulin Production:
Mutations in the INS gene can result in reduced or completely absent insulin production.
These genetic changes often interfere with the transcription or translation of the insulin gene, leading to insufficient insulin synthesis.
For instance, nonsense mutations introduce premature stop codons, truncating the insulin protein and rendering it nonfunctional.
A study in The Journal of Clinical Investigation (Edghill et al., 2008) highlighted how specific INS mutations lead to reduced insulin levels, causing severe hyperglycemia in neonates.
Without adequate insulin, glucose uptake by cells is impaired, resulting in persistent high blood sugar levels.
Protein Misfolding and ER Stress:
Many INS mutations lead to misfolded insulin proteins, which accumulate in the endoplasmic reticulum (ER) of pancreatic beta cells.
This accumulation triggers ER stress, a condition that activates the unfolded protein response (UPR) to mitigate cellular damage.
However, chronic ER stress can lead to beta-cell apoptosis, further reducing insulin production.
For example, missense mutations like C96Y disrupt the formation of disulfide bonds in proinsulin, resulting in improper folding.
Research published in Nature Medicine (Ron & Walter, 2007) explains how prolonged ER stress contributes to beta-cell failure, exacerbating neonatal diabetes.
Disrupted Insulin Secretion Pathways:
Even when insulin is produced, INS mutations can disrupt its processing and secretion pathways. Proinsulin must undergo precise enzymatic cleavage to become active insulin.
Mutations that alter this process lead to the accumulation of dysfunctional insulin precursors, which are ineffective in lowering blood glucose levels.
A study in Diabetes (Støy et al., 2007) demonstrated how specific mutations hinder insulin maturation and secretion, directly contributing to the pathophysiology of neonatal diabetes.
Types of INS Gene Mutations
Mutations in the INS gene significantly disrupt insulin production, processing, and secretion, leading to neonatal diabetes.
These mutations are classified into different types based on their genetic and functional consequences.
Missense Mutations:
Missense mutations occur when a single nucleotide change leads to the substitution of one amino acid with another.
For example, the R89C mutation replaces arginine with cysteine in the insulin molecule, disrupting the formation of critical disulfide bonds necessary for proper insulin folding.
This misfolding triggers endoplasmic reticulum (ER) stress, impairing beta-cell function and leading to reduced insulin secretion.
A study in The Journal of Clinical Investigation (Edghill et al., 2008) highlighted that missense mutations are a leading cause of beta-cell apoptosis in neonatal diabetes.
Frameshift Mutations:
Frameshift mutations result from insertions or deletions of nucleotides, altering the reading frame of the gene.
These mutations produce aberrant proinsulin proteins that are either nonfunctional or toxic to beta cells. The G32fsdelC mutation, as described in Human Mutation (Molven et al., 2008), is a prime example.
This mutation leads to the production of truncated insulin proteins that accumulate in beta cells, exacerbating cellular stress and impairing insulin secretion.
Dominant-Negative Mutations:
Dominant-negative mutations are among the most severe, as the defective protein interferes with the function of normal insulin produced by the unaffected allele.
These mutations disrupt both insulin production and secretion, often leading to persistent and severe neonatal diabetes.
Patients with dominant-negative mutations typically present with early-onset hyperglycemia that requires lifelong intervention.
Understanding these mutation types provides insight into the diverse mechanisms through which INS gene disruptions lead to neonatal diabetes, emphasizing the importance of targeted genetic screening and diagnosis.
The Unusual Case of Emma and the Twins
We would walk you through 2 such examples:
Genetic Diagnosis in a Newborn:
Emma, a three-month-old infant, was brought to the clinic with persistent hyperglycemia, severe dehydration, and failure to thrive—classic symptoms of neonatal diabetes.
Initial tests ruled out autoimmune causes, leading her pediatrician to suspect a genetic basis for her condition. Genetic testing revealed a missense mutation in the INS gene, specifically the R89H mutation.
This mutation altered the amino acid sequence of insulin, disrupting its folding process and triggering endoplasmic reticulum (ER) stress.
The accumulated misfolded proteins caused significant beta-cell apoptosis, leading to a sharp decline in insulin production.
Thanks to the early genetic diagnosis, Emma’s treatment plan was tailored to her specific condition. She transitioned from regular insulin injections to sulfonylureas, a class of drugs known to stimulate insulin secretion.
Within weeks, her blood glucose levels stabilized, and her weight gain improved.
Emma’s case highlights the transformative power of precision medicine in managing neonatal diabetes. It underscores the critical importance of genetic testing in identifying the root cause and optimizing treatment strategies for affected infants.
Familial INS Mutations:
In a family with a history of diabetes, two siblings presented with permanent neonatal diabetes mellitus (PNDM) caused by a frameshift mutation in the INS gene, specifically the G32fsdelC mutation.
The elder sibling was diagnosed at birth with severe hyperglycemia, requiring intensive insulin therapy. Learning from this experience, the family opted for genetic screening during pregnancy with their second child.
The testing confirmed the same mutation, enabling immediate intervention post-birth.
Thanks to early detection, the second sibling was started on sulfonylureas shortly after delivery, avoiding the complications that delayed treatment had caused for the older child.
The family’s story illustrates the heritable nature of some INS mutations and emphasizes the importance of familial genetic screening.
By identifying high-risk mutations early, complications can be minimized, and children can achieve better health outcomes.
This case underscores how understanding familial patterns can guide proactive healthcare in neonatal diabetes.
FAQs on Genetic Mutations in INA Genes & Neonatal Diabetes
Q1: How do mutations in the INS gene lead to neonatal diabetes?
A1: Mutations in the INS gene, which encodes insulin, can disrupt the normal folding and processing of proinsulin. This misfolding leads to the accumulation of unfolded proteins in the endoplasmic reticulum (ER), causing ER stress. The stress response can impair insulin secretion and even result in beta-cell apoptosis, contributing to neonatal diabetes.
Q2: What are the specific effects of INS gene mutations on insulin biosynthesis?
A2: INS gene mutations can decrease insulin biosynthesis through various mechanisms:
-
Translation Initiation Disruption: Mutations at the translation initiation codon can prevent the synthesis of preproinsulin.
-
mRNA Stability Reduction: Alterations in the 3′ untranslated region (UTR) can destabilize insulin mRNA, leading to reduced insulin production.
-
Transcriptional Impairment: Mutations in promoter regions can decrease the transcription of the INS gene, resulting in lower insulin levels.
Q3: How do INS gene mutations affect proinsulin processing?
A3: Certain mutations in the INS gene can lead to the production of proinsulin molecules that are misfolded or improperly processed. This misprocessing can cause the accumulation of proinsulin intermediates, which may not be efficiently converted to active insulin. The accumulation of these intermediates can further exacerbate ER stress and impair insulin secretion.
Q4: Are there specific INS gene mutations associated with neonatal diabetes?
A4: Yes, several mutations in the INS gene have been linked to neonatal diabetes. For example, mutations that alter the proinsulin molecule’s structure can prevent proper folding and processing, leading to beta-cell dysfunction. Additionally, mutations affecting the promoter region can reduce gene expression, resulting in insufficient insulin production.
Q5: How do INS gene mutations impact beta-cell function in neonates?
A5: INS gene mutations can impair beta-cell function by disrupting insulin synthesis and secretion. The accumulation of misfolded proinsulin can induce ER stress, leading to beta-cell apoptosis. Furthermore, these mutations can cause beta-cell dedifferentiation, characterized by the loss of insulin expression and the acquisition of a less differentiated state, further compromising insulin production and secretion.
Takeaway
These genetic alterations can lead to severe consequences for pancreatic beta-cell function by inducing endoplasmic reticulum (ER) stress, impairing the proper processing of proinsulin into functional insulin, or acting in a dominant-negative manner, where defective insulin interferes with normal production.
Such disruptions result in persistent hyperglycemia, a hallmark of neonatal diabetes.
Groundbreaking studies, including those published in Diabetologia and Nature Medicine, have illuminated these underlying mechanisms, offering a clearer understanding of how INS mutations contribute to this rare condition.
This growing body of research highlights the importance of identifying genetic mutations early to enable targeted interventions.
Real-world cases reinforce the critical need for early genetic diagnosis and personalized treatment plans.
While INS mutations cannot be corrected, insights gained from studying their impact pave the way for innovative therapeutic approaches.
For instance, transitioning affected individuals from insulin injections to sulfonylureas has proven successful in some cases, offering improved glycemic control.
These findings underline the importance of continued investment in neonatal diabetes research, as understanding the genetic roots of the condition is essential for developing more effective management strategies and ultimately improving patient outcomes.
References: