How HNF1A Mutations Influence MODY Development?
- admin
- November 26, 2024
- 5:37 pm
- No Comments

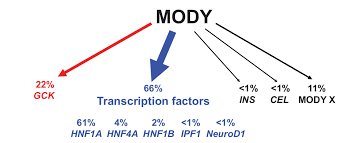
Maturity-Onset Diabetes of the Young (MODY) is a distinct, monogenic form of diabetes often misdiagnosed as Type 1 or Type 2 diabetes.
Among the genes implicated in MODY, HNF1A (Hepatocyte Nuclear Factor-1 Alpha) mutations are the most common cause of MODY3, the predominant subtype.
These mutations disrupt insulin secretion and glucose metabolism, leading to early-onset diabetes, often before age 25.
Understanding the role of HNF1A in beta-cell function and how its mutations contribute to MODY is critical for improving diagnosis and tailoring treatments.
In this article, BestDietarySupplementforDiabetics shall explore the “how” and “why” behind HNF1A mutations and their impact on MODY development.
From the gene’s role in insulin production to real-life case studies, we shall unravel the science step-by-step.
Article Index:
- What Causes MODY3 Diabetes?
- The Role of HNF1A in Glucose Regulation
- How HNF1A Mutations Affect Insulin Secretion
- Genetic Variants and Epigenetic Interactions in MODY3
- What is the Difference Between MODY and Type 1 Diabetes?
- Real-Life Case Study: Sarah’s Diagnosis of MODY3
- Best Treatment Options for HNF1A-Related MODY
- Impact of HNF1A Mutations on Pregnancy and Offspring
- Advances in Genetic Testing and Diagnosis
- FAQs on HNF1A Mutations and MODY
- How Lifestyle Factors Influence HNF1A Mutations
What Causes MODY3 Diabetes?
MODY3 results from autosomal dominant mutations in the HNF1A gene.
These mutations impair the transcription factor’s ability to regulate the genes involved in beta-cell function and glucose metabolism.
Unlike Type 1 diabetes, which involves autoimmune beta-cell destruction, or Type 2 diabetes, which is often linked to insulin resistance, MODY3 is characterized by a direct genetic cause.
HNF1A mutations disrupt the pancreatic beta cells’ ability to sense glucose levels and release insulin appropriately.
A study published in Nature Genetics highlights that MODY3 is the most common form of MODY, accounting for approximately 30-50% of all cases globally.
The Role of HNF1A in Glucose Regulation
HNF1A (Hepatocyte Nuclear Factor 1 Alpha) is a transcription factor predominantly expressed in the liver, kidneys, and pancreatic beta cells.
It plays a pivotal role in regulating genes essential for glucose metabolism.
Among its key functions, HNF1A oversees:
- Glucose Transport: It regulates the expression of glucose transporters like GLUT2, which are vital for glucose uptake by beta cells, enabling them to sense and respond to blood sugar levels.
- Insulin Secretion: By influencing genes responsible for glucose-sensing enzymes, HNF1A ensures that beta cells secrete sufficient insulin when blood glucose rises.
- Hepatic Glucose Production: It maintains balanced glucose production in the liver, preventing excessive glucose release into the bloodstream.
When HNF1A mutations occur, these finely tuned processes are disrupted, leading to impaired glucose sensing, insufficient insulin secretion, and dysregulated hepatic glucose output.
These dysfunctions are central to the development of MODY3, making HNF1A mutations a hallmark of this condition.
Understanding these mechanisms highlights the critical role of HNF1A in maintaining metabolic equilibrium.
How HNF1A Mutations Affect Insulin Secretion?
Mutations in HNF1A hinder its ability to bind DNA and activate gene transcription, resulting in:
- Defective Glucose Sensing: Reduced expression of glucose transporters leads to inadequate beta-cell glucose uptake.
- Impaired Insulin Production: The beta cells fail to secrete sufficient insulin, even in the presence of high blood glucose.
- Accelerated Beta-Cell Apoptosis: Chronic cellular stress induced by the mutations leads to early beta-cell death.
A study in The Journal of Clinical Endocrinology & Metabolism found that patients with HNF1A mutations exhibit higher fasting blood sugar levels and a progressive decline in beta-cell function, emphasizing the gene’s role in MODY development.
Genetic Variants and Epigenetic Interactions in MODY3
HNF1A mutations vary widely, with over 400 identified variants, including missense, nonsense, and frameshift mutations.
Each mutation impacts beta-cell function differently. For instance:
- Missense Mutations: Substitute one amino acid for another, altering protein function.
- Frameshift Mutations: Create a truncated, non-functional protein, severely disrupting glucose regulation.
Epigenetics adds another layer of complexity. Maternal glucose levels during pregnancy can influence gene expression in the fetus, further increasing the risk of developing MODY3 later in life.
This interplay between genes and the environment illustrates why MODY is often familial but variably expressed.
What is the Difference Between MODY and Type 1 Diabetes?
MODY (Maturity-Onset Diabetes of the Young) is frequently misdiagnosed as Type 1 diabetes due to its early onset during adolescence or young adulthood.
However, several critical differences help differentiate the two conditions:
- Genetic Basis: MODY arises from a single gene mutation (monogenic), such as HNF1A mutations in MODY3. In contrast, Type 1 diabetes is polygenic and involves an autoimmune attack on insulin-producing beta cells.
- Insulin Dependence: Unlike Type 1 diabetes, where insulin therapy is essential from the outset, most MODY cases, including MODY3, do not require insulin initially. Instead, they often respond effectively to oral medications like sulfonylureas, which stimulate insulin secretion.
- Family History: MODY follows an autosomal dominant inheritance pattern, meaning it often appears in multiple generations within a family. This inheritance pattern makes family history a valuable diagnostic clue, as opposed to the sporadic occurrence of Type 1 diabetes.
Recognizing these distinctions is crucial to avoid unnecessary insulin therapy and to provide the most effective management strategies for individuals with MODY.
Real-Life Case Study: Sarah’s Diagnosis of MODY3
Sarah, a 26-year-old nurse, struggled with fluctuating blood sugar levels despite a healthy lifestyle.
Her father, diagnosed with diabetes in his 30s, encouraged her to undergo genetic testing. The results confirmed an HNF1A mutation.
Sarah’s diagnosis clarified her condition: MODY3, not Type 2 diabetes. Her endocrinologist prescribed sulfonylureas, which improved her glucose control significantly.
This case underscores the importance of genetic testing for atypical diabetes presentations, particularly in young patients with a strong family history.
Best Treatment Options for HNF1A-Related MODY
MODY3 patients benefit from sulfonylureas, which stimulate insulin release by bypassing the glucose-sensing defects caused by HNF1A mutations.
Unlike insulin therapy, sulfonylureas directly address the underlying pathophysiology.
Studies suggest that early intervention with these medications can slow beta-cell deterioration, improving long-term outcomes.
While insulin may be required in advanced cases, most patients with MODY3 achieve effective glucose control with oral medications.
Impact of HNF1A Mutations on Pregnancy and Offspring
HNF1A mutations don’t just affect the individual—they can significantly influence pregnancy outcomes and the health of offspring.
These mutations often lead to maternal hyperglycemia, which has a profound impact on fetal beta-cell function.
This exposure can predispose the child to glucose dysregulation later in life, increasing the risk of conditions like impaired glucose tolerance or diabetes.
The question arises: Can HNF1A mutations cause complications during pregnancy?
The answer is yes. Poorly controlled blood sugar in pregnant individuals with HNF1A mutations heightens the risk of complications such as macrosomia (large birth weight) and neonatal hypoglycemia, where the newborn experiences dangerously low blood sugar levels shortly after birth.
Effective management of maternal glucose levels is crucial to minimize these risks.
A study in Diabetes Care emphasizes the importance of monitoring blood sugar closely during pregnancy and tailoring treatment to the unique challenges posed by MODY3, ensuring better outcomes for both mother and baby.
FAQs on HNF1A Mutations and MODY
Q-1: How does an HNF1A mutation turn a normal β-cell into a “late responder”?
A-1: HNF1A is a transcription hub for glucose sensing and stimulus–secretion coupling. When it is impaired, β-cells underexpress key transporters and enzymes, so ATP rises sluggishly after meals. KATP channels stay open longer, calcium entry lags, and the first-phase insulin burst is muted. Clinically, post-meal glucose climbs higher and longer, even when fasting values look near-normal early on.
Q-2: Why do families with HNF1A variants show diabetes across generations—but with different severities?
A-2: HNF1A-MODY is autosomal dominant, yet penetrance and severity vary. Puberty, pregnancy, intercurrent illness, and polygenic background can unmask or amplify the secretion defect at different ages. One relative might have mild, diet-responsive hyperglycemia for years; another, with the same variant, needs medication in their teens. The gene sets the risk, while life-stage stressors and modifiers tune the phenotype.
Q-3: What non-pancreatic “fingerprints” suggest HNF1A is the culprit before genetic testing?
A-3: Three handy clues: (1) Low renal glucose threshold—glycosuria appears at relatively modest glucose levels due to reduced tubular reabsorption; (2) Persistently low hs-CRP for the degree of hyperglycemia because HNF1A regulates hepatic CRP expression; (3) Preserved C-peptide years after diagnosis with negative islet autoantibodies. Together with a vertical family pattern and early onset, these point strongly toward HNF1A-driven MODY.
Q-4: How do HNF1A mutations shape treatment choices differently from Type 1 or Type 2 diabetes?
A-4: Because the downstream release machinery remains intact, low-dose sulfonylureas often restore a robust insulin pulse by directly closing KATP channels—bypassing the faulty glucose-sensing step. Doses are typically much smaller than in Type 2, and hypoglycemia education matters. Many individuals can de-escalate or avoid insulin when correctly classified, while lifestyle support (protein-forward meals, regular activity) improves durability of control.
Q-5: What special considerations apply in pregnancy and long-term follow-up for HNF1A-MODY?
A-5: Preconception planning is key: some oral agents cross the placenta, so insulin is commonly preferred during pregnancy. Family cascade testing clarifies fetal considerations and future risk for relatives. Long term, monitor lipids, kidney function, and microvascular risk as glycemia evolves with age or life events. If glucose control shifts, reassess therapy rather than assuming “Type 2 drift”—the underlying biology remains an insulin-secretion defect rooted in HNF1A.
Advances in Genetic Testing and Diagnosis
Genetic testing has become the definitive approach for diagnosing MODY, especially MODY3 caused by HNF1A mutations.
Advances in sequencing technologies, such as next-generation sequencing (NGS) panels, allow for precise and efficient identification of genetic variants linked to the condition.
Early diagnosis through genetic testing offers several advantages:
- Tailored Treatment: Identifying the exact mutation enables healthcare providers to recommend appropriate treatments, such as sulfonylureas, over standard diabetes management strategies.
- Avoiding Misdiagnosis: Genetic testing differentiates MODY3 from Type 1 or Type 2 diabetes, reducing unnecessary insulin prescriptions and avoiding the complications of mismanagement.
- Cascade Testing: Once a mutation is identified, family members can undergo testing to assess their risk, enabling early intervention if necessary.
Patients often wonder, “How does genetic testing diagnose MODY?” The answer lies in its ability to pinpoint specific mutations that disrupt glucose regulation, providing clarity for both diagnosis and treatment.
How Lifestyle Factors Influence HNF1A Mutations?
While HNF1A mutations form the genetic basis of MODY3, environmental factors such as diet and exercise significantly influence its development and progression.
Poor lifestyle choices, including high-calorie diets and sedentary behavior, can worsen the effects of these mutations by increasing insulin resistance and placing additional stress on pancreatic beta cells.
This interplay between genetics and environment raises the question, “Why is MODY3 the most common MODY type?”
One possible explanation lies in how prevalent lifestyle factors, such as unhealthy eating and limited physical activity, amplify the metabolic challenges posed by HNF1A mutations.
These environmental triggers may contribute to its higher occurrence compared to other MODY types.
The good news is that addressing these factors can positively impact disease management.
Studies have shown that adopting a balanced diet and engaging in regular exercise not only improve glucose control but also help delay the progression of MODY3.
Conclusion
HNF1A mutations significantly influence MODY development by impairing beta-cell function and disrupting glucose metabolism.
Understanding the genetic and epigenetic mechanisms involved allows for precise diagnosis and treatment, ensuring better outcomes for patients.
Through genetic testing, personalized treatment plans, and lifestyle modifications, individuals with MODY3 can achieve effective glucose control and a better quality of life.
By integrating advanced research and clinical care, the future looks promising for those affected by HNF1A mutations.
References: