How HNF1B Mutations Impair Insulin Production?
- admin
- December 7, 2024
- 9:18 am
- No Comments
Hepatocyte nuclear factor 1-beta (HNF1B) is a crucial transcription factor involved in the development and functioning of various organs, including the pancreas, kidneys, and liver.
It plays a significant role in regulating genes essential for insulin production, and mutations in the HNF1B gene can disrupt this process, leading to impaired insulin synthesis and secretion.
This dysfunction is a key factor in specific forms of diabetes, such as maturity-onset diabetes of the young type 5 (MODY5).
In this article, we will explore the mechanisms by which HNF1B mutations impair insulin production, discuss the clinical manifestations, and provide real-life examples to illustrate these concepts.
Table of Contents:
- Introduction to HNF1B and Its Role in Insulin Production
- Mechanisms of Impaired Insulin Production Due to HNF1B Mutations
- 2.1. Disruption of Pancreatic Development
- 2.2. β-Cell Dysfunction and Insulin Secretion Impairment
- 2.3. Altered Gene Expression in Insulin Production Pathways
- Clinical Manifestations of HNF1B Mutations
- 3.1. MODY5: The Diabetes Linked to HNF1B Mutations
- 3.2. Extrapancreatic Manifestations and Multisystem Involvement
- Real-Life Examples of HNF1B Mutations and Diabetes
- 4.1. Case Study: Early-Onset Diabetes in a Young Adult
- 4.2. Case Study: A Family History of MODY5
- Conclusion
Introduction to HNF1B and Its Role in Insulin Production
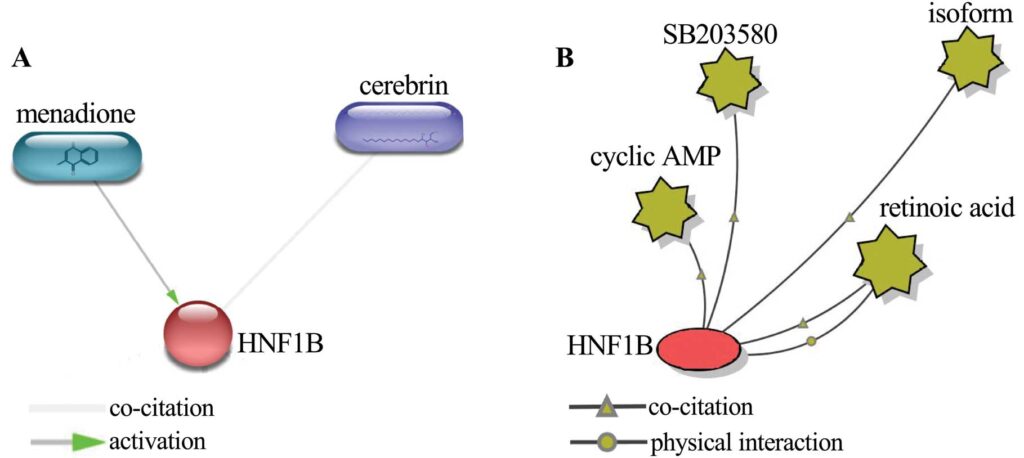
HNF1B is a nuclear transcription factor that controls the expression of numerous genes essential for the normal functioning of pancreatic β-cells.
These cells are responsible for producing insulin, the hormone required to regulate blood glucose levels.
HNF1B is not only critical during the development of the pancreas but also plays a key role in maintaining β-cell health and function in adulthood.
Proper HNF1B activity ensures that the pancreas has an adequate β-cell mass and that these cells can respond appropriately to rising blood glucose levels by secreting insulin.
When HNF1B mutations occur, this finely balanced system is disrupted.
These mutations can lead to structural abnormalities in the pancreas, β-cell dysfunction, and impaired gene regulation, all of which negatively impact insulin production.
Understanding how and why these mutations impair insulin production is critical for diagnosing and managing conditions like MODY5.
Mechanisms of Impaired Insulin Production Due to HNF1B Mutations
HNF1B mutations impair insulin production through a combination of developmental, functional, and genetic disruptions.
These mechanisms explain why individuals with these mutations often develop diabetes.
Disruption of Pancreatic Development:
HNF1B plays a pivotal role during embryonic development, particularly in the formation of the pancreas. Mutations in this gene can result in pancreatic hypoplasia (underdeveloped pancreas) or, in severe cases, pancreatic agenesis (absence of the pancreas).
Both conditions lead to a significant reduction in the β-cell population, which directly decreases the body’s ability to produce insulin.
A study published in Diabetes Research and Clinical Practice (Faguer et al., 2011) highlighted that individuals with HNF1B mutations often exhibit structural abnormalities in the pancreas.
These abnormalities are frequently detected through imaging studies and are a hallmark of MODY5. In cases of hypoplasia, the reduced β-cell mass translates into insufficient insulin production, making it difficult to maintain normal glucose levels.
β-Cell Dysfunction and Insulin Secretion Impairment:
Even in cases where the pancreas appears structurally normal, HNF1B mutations can impair the function of β-cells.
β-cell dysfunction occurs because HNF1B is involved in the regulatory pathways that control glucose-stimulated insulin secretion.
Mutations in HNF1B disrupt these pathways, leading to an insufficient release of insulin in response to rising blood glucose levels.
Research from Endocrine Reviews (Edghill et al., 2008) demonstrated that individuals with HNF1B mutations exhibit lower β-cell activity compared to healthy individuals.
This dysfunction is a major contributing factor to the hyperglycemia observed in MODY5 patients, as their insulin response is inadequate to manage postprandial glucose spikes.
Altered Gene Expression in Insulin Production Pathways:
HNF1B regulates the expression of multiple genes essential for β-cell function, including those directly involved in insulin synthesis and secretion.
Mutations in HNF1B alter its transcriptional activity, reducing the expression of critical genes such as insulin and glucose transporter type 2 (GLUT2).
This impairment leads to decreased insulin synthesis and an inability of β-cells to respond effectively to glucose stimuli.
A study published in Nature Genetics (Bingham et al., 2001) highlighted how HNF1B mutations disrupt the transcription of genes essential for glucose metabolism and insulin production.
This finding underscores the importance of HNF1B in maintaining β-cell functionality and explains why mutations in this gene lead to impaired insulin production.
Clinical Manifestations of HNF1B Mutations
HNF1B mutations result in distinct clinical conditions, with MODY5 being the most well-recognized manifestation.
However, these mutations can also lead to extrapancreatic complications.
MODY5: The Diabetes Linked to HNF1B Mutations:
MODY5 is a rare form of monogenic diabetes caused by HNF1B mutations.
It is characterized by early-onset diabetes, typically before the age of 25, and is inherited in an autosomal dominant pattern.
Unlike type 1 or type 2 diabetes, MODY5 is primarily caused by impaired β-cell function rather than autoimmunity or insulin resistance.
Individuals with MODY5 often present with mild hyperglycemia, which may progress to overt diabetes if not managed.
A review in Diabetes Care (Hattersley et al., 2018) emphasized that the underlying β-cell dysfunction in MODY5 is a direct result of HNF1B mutations, making genetic testing crucial for accurate diagnosis.
Extrapancreatic Manifestations and Multisystem Involvement:
HNF1B mutations are not limited to the pancreas; they also affect other organs, leading to multisystem involvement.
Renal abnormalities, such as renal cysts, structural anomalies, and chronic kidney disease, are common in individuals with HNF1B mutations.
Other complications may include genital tract malformations, electrolyte imbalances, and liver dysfunction.
The Journal of Clinical Endocrinology & Metabolism (Faguer et al., 2011) highlighted that the extrapancreatic manifestations of HNF1B mutations often precede the diagnosis of diabetes.
Recognizing these signs is essential for early detection and intervention.
Real-Life Cases Provide Practical Insights into HNF1B Mutations and Insulin Impairment
Real-life examples offer valuable understanding of how HNF1B mutations impair insulin production and affect patients’ lives.
These cases illustrate the variability in clinical presentation and highlight the importance of early diagnosis and personalized treatment strategies.
Case Study: Early-Onset Diabetes in a Young Adult
A 22-year-old male visited his physician for a routine check-up and was found to have persistent hyperglycemia.
Despite his efforts to maintain a healthy diet and active lifestyle, his fasting blood glucose levels were consistently elevated.
He had no significant family history of type 1 or type 2 diabetes, and autoimmune testing ruled out type 1 diabetes.
Further investigation using imaging studies revealed mild pancreatic hypoplasia—a condition where the pancreas is underdeveloped, limiting its capacity for insulin production.
To pinpoint the cause of his diabetes, genetic testing was conducted and identified a mutation in the HNF1B gene.
Based on the findings, he was diagnosed with MODY5, a monogenic form of diabetes linked to β-cell dysfunction due to HNF1B mutations.
The patient was started on sulfonylurea therapy, a class of medications that stimulates insulin secretion from β-cells.
His blood glucose levels improved significantly with this tailored treatment approach.
This case emphasizes the importance of considering genetic factors in young individuals presenting with unexplained hyperglycemia, especially when traditional diabetes types are ruled out.
Case Study: A Family History of MODY5
In another example, a family spanning three generations showed a consistent pattern of early-onset diabetes.
Multiple family members also exhibited renal abnormalities, such as cystic kidney disease, in addition to elevated blood glucose levels.
These findings prompted genetic testing, which revealed a shared mutation in the HNF1B gene among affected individuals.
The diagnosis confirmed MODY5 as the underlying cause of their diabetes and renal involvement.
The family members displayed variable clinical presentations.
While some required insulin therapy to manage their blood sugar levels, others maintained adequate control with dietary modifications and oral medications.
This variability underscores the diverse impact of HNF1B mutations, even within the same family.
The autosomal dominant inheritance pattern observed in this case highlights the importance of family screening when HNF1B mutations are suspected.
Early identification of at-risk relatives allowed for proactive monitoring and intervention, improving long-term outcomes.
These real-life cases demonstrate the profound impact of HNF1B mutations on insulin production and their broader implications.
They underline the critical role of genetic testing in diagnosing and managing conditions like MODY5 and illustrate the need for individualized treatment strategies tailored to each patient’s unique presentation.
Conclusion
HNF1B mutations impair insulin production through mechanisms that include disrupted pancreatic development, β-cell dysfunction, and altered gene expression.
These mutations lead to clinical conditions such as MODY5 and are often accompanied by extrapancreatic complications.
Early recognition of HNF1B mutations, through genetic testing and clinical evaluation, is crucial for accurate diagnosis and effective management.
Real-life examples demonstrate the profound impact of these mutations on patients’ lives and highlight the need for personalized treatment approaches.
As research advances, understanding the molecular mechanisms of HNF1B mutations will pave the way for targeted therapies to improve outcomes for affected individuals.
References: