How Hormones Trigger Gestational Diabetes: What Every Mom Needs to Know
- admin
- September 16, 2024
- 11:07 am
- No Comments

Pregnancy is an exciting and life-changing time, but it is also when your body undergoes significant hormonal changes to support the growth and development of your baby.
These hormonal shifts, while essential, can sometimes lead to unexpected health conditions like gestational diabetes.
Gestational diabetes is a type of diabetes that occurs during pregnancy, typically in the second or third trimester, when your body becomes less responsive to insulin.
But what’s causing this insulin resistance?
The answer lies in the gestational diabetes hormone—a key factor in pregnancy-related changes.
In particular, human placental lactogen (HPL) plays a major role in how your body manages blood sugar levels.
This article will explain how hormones, especially those related to the placenta, trigger gestational diabetes and what every expectant mother should know to manage the condition.
Contents of “How Hormones Trigger Gestational Diabetes” Article:
- What is Gestational Diabetes?
- How Hormones Contribute to Gestational Diabetes
- Human Placental Lactogen and Gestational Diabetes: The Connection
- Other Placental Hormones That Affect Blood Sugar
- Signs and Symptoms of Gestational Diabetes
- Managing and Preventing Gestational Diabetes
- Conclusion: Understanding the Role of Hormones in Gestational Diabetes
What is Gestational Diabetes?
Gestational diabetes is a condition that affects pregnant women, typically in the latter half of their pregnancy.
It occurs when the body becomes less sensitive to insulin, a hormone that helps regulate blood sugar. Insulin allows glucose to enter cells, providing energy for both the mother and the growing baby.
When insulin resistance occurs, blood sugar levels rise, leading to gestational diabetes.
Unlike type 1 or type 2 diabetes, gestational diabetes usually resolves after pregnancy. However, it’s essential to manage this condition during pregnancy to avoid complications for both the mother and baby.
According to the American Diabetes Association, around 6% to 9% of pregnant women in the U.S. develop gestational diabetes, making it one of the most common complications during pregnancy.

How Hormones Contribute to Gestational Diabetes?
Hormones are crucial in pregnancy, supporting everything from the baby’s development to the mother’s changing body.
However, these hormones can also interfere with insulin’s ability to regulate blood sugar, leading to insulin resistance.
The placental hormones gestational diabetes connection is particularly significant, as the placenta produces various hormones that alter insulin sensitivity.
One of the primary hormones involved is human placental lactogen (HPL), also known as human chorionic somatomammotropin.
Produced by the placenta, HPL plays a vital role in regulating the metabolism of the mother and ensuring the baby gets enough glucose for growth.
However, this hormone also contributes to insulin resistance, increasing blood sugar levels.
Human Placental Lactogen and Gestational Diabetes: The Connection
Human placental lactogen (HPL) is a hormone that becomes more active as pregnancy progresses, reaching its peak in the third trimester.
Its primary function is to promote milk production and regulate the mother’s metabolism.
HPL increases the amount of glucose available to the baby by reducing the mother’s sensitivity to insulin. This action ensures that the baby receives enough energy for growth and development.
While this process is necessary for the baby, it can create challenges for the mother. As HPL levels rise, the body becomes less effective at using insulin, leading to elevated blood sugar levels—a hallmark of gestational diabetes.
In fact, the link between HPL and gestational diabetes is well-established in medical literature, with studies highlighting how rising levels of human placental lactogen contribute to the development of human placental lactogen diabetes.
Other Placental Hormones That Affect Blood Sugar
In addition to HPL, other placental hormones also play a role in gestational diabetes. These include:
- Progesterone: This hormone supports the uterine lining and helps maintain pregnancy. However, it can also contribute to insulin resistance by interfering with insulin’s ability to transport glucose into cells.
- Estrogen: While estrogen is critical for the development of both the placenta and the baby, it also impacts insulin sensitivity. High levels of estrogen can make it harder for the mother’s body to effectively manage blood sugar levels.
- Cortisol: Often referred to as the “stress hormone,” cortisol increases during pregnancy and can raise blood sugar levels. While cortisol helps the body cope with physical stress, it can also exacerbate insulin resistance, further increasing the risk of gestational diabetes.
Together, these placental hormones gestational diabetes contributions make it clear that hormonal changes are a central cause of gestational diabetes.
Signs and Symptoms of Gestational Diabetes
While hormonal changes are the root cause, recognizing the signs and symptoms of gestational diabetes is crucial for early detection and management.
Common symptoms include:
- Increased thirst: Gestational diabetes can cause elevated blood sugar levels, leading to dehydration and increased thirst.
- Frequent urination: Higher blood sugar levels can make your kidneys work harder, leading to more frequent trips to the bathroom.
- Fatigue: While fatigue is common during pregnancy, extreme tiredness could signal gestational diabetes, as the body struggles to manage high blood sugar levels.
- Blurred vision: Elevated blood sugar can affect fluid levels in the eyes, causing blurred vision.
- Unexplained weight loss: In some cases, gestational diabetes can cause the body to burn fat for energy, leading to unintentional weight loss.
If you experience any of these symptoms, it is essential to speak with your healthcare provider. Regular screenings, including glucose tolerance tests, are typically conducted during pregnancy to identify gestational diabetes.
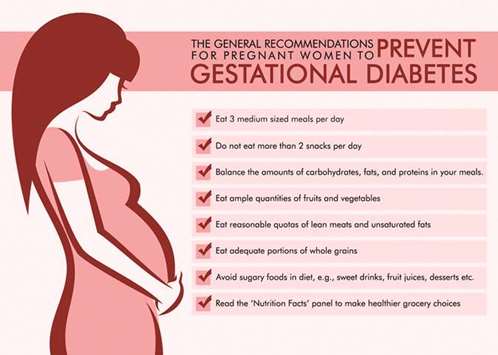
Managing and Preventing Gestational Diabetes
The good news is that gestational diabetes can often be managed with lifestyle changes, and in some cases, medication.
Here is how you can reduce your risk or manage the condition if diagnosed:
- Healthy diet: Focusing on a balanced diet that includes complex carbohydrates, lean proteins, and healthy fats can help regulate blood sugar levels. Limiting sugary foods and refined carbohydrates is key. Adding natural Supplements to Lower Blood Sugar are highly recommended.
- Regular exercise: Physical activity improves insulin sensitivity and helps regulate blood sugar. Walking, swimming, and prenatal yoga are excellent options for pregnant women.
- Monitoring blood sugar: If diagnosed with gestational diabetes, regular blood sugar checks are necessary to ensure that levels remain within a healthy range.
- Medication: In some cases, diet and exercise alone may not be enough. Your doctor may prescribe insulin or other medications to help manage blood sugar levels.
A 2018 study published in The Journal of Maternal-Fetal & Neonatal Medicine found that women who managed their gestational diabetes through diet and exercise had better pregnancy outcomes and reduced complications compared to those who did not make these lifestyle changes.
Understanding the Role of Hormones in Gestational Diabetes – Conclusive Analysis
So, how do hormones trigger gestational diabetes, and what should every expectant mom know?
The answer lies in the complex relationship between pregnancy hormones and insulin resistance.
Hormones like human placental lactogen play a vital role in supporting the baby’s growth, but they also reduce the mother’s ability to process glucose efficiently. As a result, blood sugar levels can rise, leading to gestational diabetes.
Understanding the hormonal triggers behind gestational diabetes helps expectant mothers take proactive steps to manage the condition.
While gestational diabetes can be a challenging part of pregnancy, it’s important to remember that with proper management, the risks to both mother and baby can be minimized.
By focusing on healthy habits, staying active, and working with your healthcare team, you can have a healthy and successful pregnancy.
References: