How Insulin Dysregulation Leads to Type 2 Diabetes?
- admin
- October 12, 2024
- 7:28 pm
- No Comments
I did not think much about insulin until my routine health check-up flagged my blood sugar levels.
Like many others, I believed diabetes was something that happened to someone else or much later in life.
But as I learned more about how my body processes food, I discovered that insulin plays a critical role in keeping blood sugar stable—and when this delicate balance falters, it can set the stage for type 2 diabetes.
Insulin dysregulation is often an invisible process, one that can go unnoticed until it causes significant issues like type 2 diabetes.
It occurs when the body’s cells stop responding efficiently to insulin, or the pancreas can no longer produce enough insulin to maintain healthy blood sugar levels.
In this article, bestdietarysupplementfordiabetics.com would find out how and why insulin dysregulation leads to type 2 diabetes, focusing on the physiological mechanisms, lifestyle factors, and how daily habits can accelerate or slow down the onset of this condition.
In This Article:
- What is Insulin and How Does It Work?
- Understanding Insulin Dysregulation: The First Step Toward Type 2 Diabetes
- How Lifestyle Choices Contribute to Insulin Dysregulation
- The Role of Insulin Resistance in Type 2 Diabetes
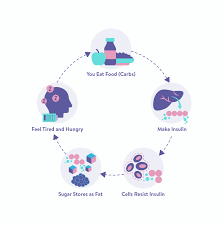
- The Vicious Cycle of High Blood Sugar and Insulin Dysregulation
- Real-Life Examples: How Daily Habits Can Lead to Insulin Dysregulation
- FAQs on Insulin Dysregulation & Type 2 Diabetes
- Conclusion: How Insulin Dysregulation Leads to Type 2 Diabetes
What is Insulin and How Does It Work?
Before diving into insulin dysregulation, let us start with the basics.
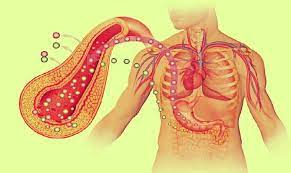
Insulin is a hormone produced by the pancreas that plays a critical role in regulating blood sugar levels.
When you eat, your body breaks down carbohydrates into glucose, which enters your bloodstream. As blood sugar levels rise, the pancreas releases insulin to help move glucose from the bloodstream into your cells, where it can be used for energy.
Think of insulin as a key that unlocks your cells so they can absorb glucose. Without enough insulin or if your body becomes resistant to it, blood sugar levels remain elevated, which can cause damage to organs and tissues over time.
I started paying attention to this process when I found myself frequently tired after meals. I assumed I was not getting enough sleep, but it was actually a sign that my cells were not absorbing glucose effectively, a classic symptom of insulin dysregulation.
Understanding Insulin Dysregulation: The First Step Toward Type 2 Diabetes
Insulin dysregulation is often the silent spark that ignites the slow burn toward type 2 diabetes. It refers to the breakdown in the finely tuned relationship between insulin production and glucose usage in your body.
When this system falters, blood sugar levels can begin to climb—even before diabetes is officially diagnosed.
There are two major culprits behind insulin dysregulation: insulin resistance and insufficient insulin production. Insulin resistance means that your cells no longer respond effectively to insulin’s signals.
This is particularly common in people with sedentary lifestyles, excess abdominal fat, and chronic inflammation.
To compensate, the pancreas ramps up insulin production—sometimes producing 2 to 3 times the normal amount. However, this compensation can only go so far before the pancreatic beta cells start to fail.
On the flip side, insufficient insulin production may result from long-term overuse of the pancreas, often driven by years of compensating for insulin resistance. The beta cells begin to “burn out,” leading to reduced insulin output.
According to the Journal of Clinical Endocrinology & Metabolism, nearly 50% of beta-cell function may already be lost by the time type 2 diabetes is diagnosed.
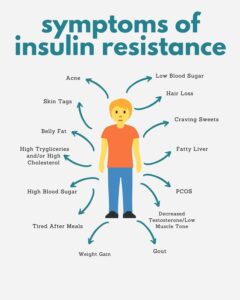
The earliest signs of insulin dysregulation can be deceptive. I noticed persistent fatigue, uncontrollable sugar cravings, and unexplained weight gain—classic early indicators. Many people dismiss these as aging or stress, but they reflect deeper metabolic issues.
Studies show that even mild hyperinsulinemia (excess insulin in the blood) is associated with higher risks of obesity, PCOS, fatty liver disease, and cardiovascular complications.
Another key factor is chronically elevated insulin levels, which can precede glucose changes by years. According to a 2022 review in Diabetes Care, fasting insulin levels are often elevated 5–10 years before any noticeable rise in fasting glucose.
This means insulin resistance starts damaging your health long before your blood sugar spikes.
Understanding these early shifts is crucial. Detecting insulin dysregulation through tests like fasting insulin, HOMA-IR index, or even post-meal glucose readings can offer a life-changing head start—often years before type 2 diabetes officially arrives
How Lifestyle Choices Contribute to Insulin Dysregulation?
One of the most important factors contributing to insulin dysregulation is lifestyle.
What we eat, how active we are, and even how we manage stress can all influence how effectively our bodies use insulin.
Here is a closer look at how daily habits play a role:
-
Diet: A diet high in refined carbohydrates and sugars can cause repeated spikes in blood sugar, forcing the pancreas to pump out more insulin. Over time, this can lead to insulin resistance. For example, indulging in sugary snacks or processed foods causes rapid glucose spikes, requiring your body to release higher amounts of insulin. I realized that my frequent sugary snacks were more harmful than I thought, leading to constant fluctuations in blood sugar.
-
Physical inactivity: Muscles are one of the primary tissues that absorb glucose. Regular physical activity helps your muscles stay responsive to insulin, allowing glucose to be used for energy. When you’re sedentary, your body becomes less efficient at using insulin, leading to dysregulation.
-
Chronic stress: Stress triggers the release of cortisol, a hormone that raises blood sugar levels. If you’re constantly stressed, your body has to release more insulin to manage elevated blood sugar. Over time, this can lead to insulin resistance. Personally, during stressful times, I noticed that I craved more sugary foods, and I began feeling sluggish, which I now understand was related to insulin dysregulation.
The Role of Insulin Resistance in Type 2 Diabetes
Insulin resistance is the key driver in the development of type 2 diabetes.
When your cells stop responding effectively to insulin, the pancreas compensates by producing more of the hormone to help move glucose into the cells.
However, this is only a temporary fix. Over time, the pancreas becomes overworked, and its ability to produce insulin diminishes.
This marks the beginning of type 2 diabetes, where the body cannot properly regulate blood sugar.
I found out from my doctor that my body was producing more insulin than normal, but it wasn’t enough to keep my blood sugar in check. This process was the beginning of insulin resistance for me.
Scientific studies confirm that insulin resistance is the strongest predictor of type 2 diabetes.
According to research from the Journal of Clinical Endocrinology & Metabolism, individuals with high levels of insulin resistance are significantly more likely to develop type 2 diabetes within a few years.
The problem with insulin resistance is that it often goes unnoticed. People can have it for years before they experience significant symptoms.
I learned this the hard way, as my blood sugar levels were slowly creeping up long before I noticed any obvious signs of diabetes.
The Vicious Cycle of High Blood Sugar and Insulin Dysregulation
Once insulin dysregulation sets in, it creates a vicious cycle that can be difficult to break.
Elevated blood sugar levels cause the pancreas to release more insulin, but if the cells remain resistant, blood sugar remains high, and the pancreas continues to overproduce insulin. Over time, this leads to a breakdown in the body’s ability to regulate blood sugar.
I vividly remember a period when I felt constantly tired and hungry, despite eating more than usual.
I craved carbs and sweets, not realizing that my body was struggling to regulate my blood sugar levels. This cycle made me feel even more fatigued, which in turn led to more unhealthy food choices.
As blood sugar levels stay high, they cause inflammation and damage to blood vessels and nerves, leading to complications such as heart disease, kidney failure, and neuropathy, which are common in type 2 diabetes.
Real-Life Examples: How Daily Habits Can Lead to Insulin Dysregulation
Let us take a closer look at how typical daily habits can gradually lead to insulin dysregulation and eventually type 2 diabetes:
-
Skipping breakfast: This might seem harmless, but when you skip meals, your blood sugar drops, and when you finally eat, it spikes. These fluctuations can stress the pancreas and lead to insulin resistance over time.
-
Snacking on processed foods: Frequent consumption of foods like chips, cookies, and soda leads to constant insulin release. I used to have snacks while working, and I didn’t realize that the constant grazing was forcing my body to release more insulin than needed.
-
Lack of physical activity: Sitting at a desk all day, combined with limited exercise, reduces muscle insulin sensitivity. When I became more sedentary due to work, I noticed that my energy levels dropped significantly, which is a direct result of my muscles not effectively using glucose.
-
Chronic stress: Juggling work deadlines, family responsibilities, and daily stress can take a toll on your body. I realized that during stressful periods, I craved more sugary foods, which further worsened my insulin sensitivity.
By making small changes in daily habits, such as incorporating more physical activity, reducing processed foods, and managing stress better, it is possible to prevent or delay insulin dysregulation from progressing to type 2 diabetes.
FAQs on Insulin Dysregulation & Type 2 Diabetes
Q-1: What exactly is insulin dysregulation and how does it lead to type 2 diabetes?
A-1: Insulin dysregulation occurs when the body’s normal insulin response becomes impaired, meaning insulin no longer signals cells effectively to absorb glucose.
In early stages, the pancreas produces more insulin to compensate, but cells in muscle, fat, and liver gradually become resistant to its action.
As insulin becomes less effective, blood glucose levels remain elevated for longer, forcing even greater insulin secretion.
Over time, this imbalance exhausts the pancreatic cells that make insulin and accelerates the transition from insulin resistance to progressive type 2 diabetes development.
Q-2: How does early insulin resistance disrupt normal glucose metabolism?
A-2: In a healthy system, insulin acts like a key that opens doors for glucose to enter cells.
With insulin resistance, these “doors” don’t open properly, so glucose accumulates in the bloodstream. The pancreas tries to keep up by pumping out more insulin, but this overproduction only temporarily controls blood sugar.
Persistent high glucose and high insulin levels eventually damage pancreatic cells and reduce their ability to produce insulin, contributing to impaired glucose regulation preceding diabetes.
Q-3: Can insulin dysregulation cause blood sugar spikes even when fasting?
A-3: Yes. When cells become resistant to insulin, the liver often continues releasing glucose into the blood even in the fasting state because insulin’s restraining signal weakens.
This results in elevated fasting blood glucose levels — one of the earliest measurable signs of type 2 diabetes risk — and reflects how insulin signaling failure impacts fasting glucose control.
Q-4: Why does chronic insulin dysregulation affect weight and fat distribution?
A-4: Insulin isn’t only a glucose regulator — it also influences how the body stores and uses fat. When cells resist insulin, more glucose stays in the bloodstream and less is used for energy.
The body converts excess glucose into fat, particularly around the abdomen. This abdominal fat worsens insulin resistance in a feedback loop that contributes to metabolic dysfunction and diabetes progression.
Q-5: Can improving insulin sensitivity reverse or slow the progression toward type 2 diabetes?
A-5: Yes. Enhancing insulin sensitivity through dietary changes, physical activity, weight management, and targeted lifestyle modifications helps cells respond more effectively to insulin.
Improved insulin action lowers blood glucose and reduces the burden on pancreatic cells, slowing or even partially reversing the trajectory toward type 2 diabetes onset due to insulin dysregulation.
Takeaway:
In summary, insulin dysregulation is the gateway to type 2 diabetes. It begins with insulin resistance, where the body’s cells stop responding to insulin, leading to elevated blood sugar levels.
Over time, the pancreas becomes unable to keep up with insulin production, and blood sugar levels remain chronically high, marking the onset of type 2 diabetes.
Daily lifestyle habits, such as poor diet, physical inactivity, and chronic stress, can accelerate insulin dysregulation.
Understanding how these habits influence insulin sensitivity is critical in preventing type 2 diabetes by learning how to lower blood sugar naturally.
While it is easy to overlook the early signs, paying attention to your body’s signals and making small, sustainable changes can go a long way in protecting your long-term health.
References: