How Necrosis Affects Pancreatic Tissue in Type 3c Diabetes?
- admin
- November 6, 2024
- 9:52 am
- No Comments
Necrosis, that pesky process of tissue death, does not just create havoc wherever it strikes; it can turn into a significant player in the development and worsening of type 3c diabetes.
Today, bestdietarysupplementfordiabetics shall explore this unique relationship between necrosis and the pancreas, particularly in the context of type 3c diabetes.
How does necrosis impact pancreatic tissue?
And why does it have such an influence on this less commonly discussed form of diabetes?
Buckle up; we are about to dive into the details, including how necrosis takes hold, what it does to pancreatic cells, and the various ways it alters the overall functioning of the pancreas.
Article Index:
- Understanding Necrosis and Its Impacts on the Body
- An Introduction to Type 3c Diabetes
- Necrosis in Pancreatic Tissue: Mechanisms and Causes
- The Link Between Pancreatic Necrosis and Insulin Production
- Long-term Impacts of Necrosis on Pancreatic Tissue in Type 3c Diabetes
- Real-Life Examples: How Necrosis Influences Pancreatic Functioning
- FAQS on on Necrosis and Type 3c Diabetes
- Scientific Evidence on Necrosis and Type 3c Diabetes
Understanding Necrosis and Its Impacts on the Body
Necrosis, simply put, is the process of cell death that happens when cells are so damaged they cannot be repaired.
It is not a programmed or “clean” process like apoptosis (natural cell death) but rather a chaotic one that releases harmful substances into surrounding tissues.
When necrosis strikes, inflammation tends to follow, as the immune system tries to clear out dead cells and control infection.
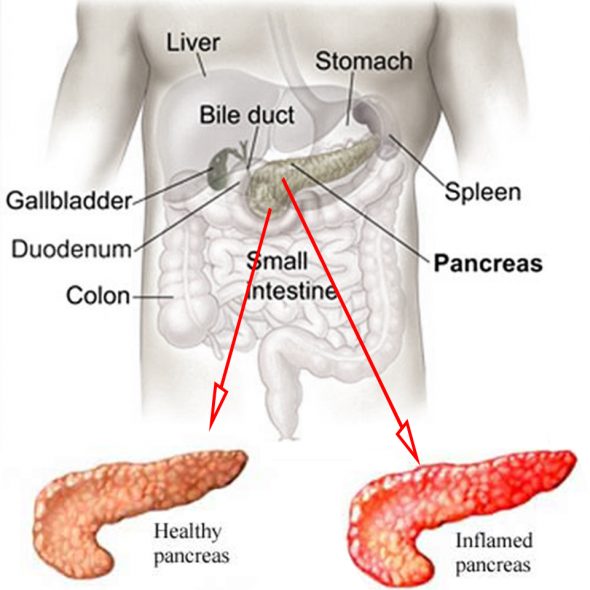
In pancreatic tissue, necrosis can be particularly problematic, as it not only damages cells essential for insulin production but also causes long-lasting inflammation.
Chronic Inflammation gives rise to type 3c diabetes. So, this is a chain reaction of sorts.
The process can start as an injury to pancreatic cells, which eventually spreads, disrupting normal cell function and leading to tissue death.
An Introduction to Type 3c Diabetes
Type 3c diabetes, also known as pancreatogenic diabetes, is a form of diabetes that results from disease or damage to the pancreas.
Unlike type 1 or type 2 diabetes, type 3c is primarily caused by the destruction or impairment of pancreatic tissue, often resulting from necrosis, inflammation, or injury due to pancreatitis, surgery, or cystic fibrosis.
In type 3c diabetes, necrosis plays a significant role in pancreatic dysfunction, impacting the pancreas’s ability to produce insulin and other enzymes.
This is because the pancreas is not just about insulin – it also produces enzymes crucial for digestion. When necrosis affects the pancreas, it impacts both these essential roles, leading to both metabolic and digestive issues.
Necrosis in Pancreatic Tissue: Mechanisms and Causes
Necrosis in pancreatic tissue can happen due to a variety of factors – from acute pancreatitis to physical injury or chronic inflammation.
When necrosis occurs, it can affect the beta cells in the pancreas, responsible for insulin production, as well as other cells involved in enzyme production.
As the tissue dies, it disrupts the normal functioning of the pancreas, making it difficult for the body to maintain balanced blood sugar levels.
Research from The Journal of Pathology highlights that necrotic cells release enzymes and inflammatory substances that can spread, damaging neighboring cells and causing more widespread pancreatic necrosis.
This chain reaction can become quite severe, leading to significant loss of pancreatic tissue, which is crucial for insulin regulation.
The Link Between Pancreatic Necrosis and Insulin Production
As necrosis spreads in pancreatic tissue, it leads to a reduction in beta cell mass.
Beta cells are like tiny insulin factories in the pancreas, and when they are damaged or destroyed, the body struggles to produce enough insulin.
Without adequate insulin, blood sugar levels rise, contributing to diabetes.
A study published in Diabetes Care explored the effects of pancreatic necrosis on beta cells often triggering MODY, concluding that this destruction results in decreased insulin production and release.
The inflammation caused by necrosis also interferes with beta cell function, further reducing insulin output and leading to the glucose imbalances typical of diabetes.
Long-term Impacts of Necrosis on Pancreatic Tissue in Type 3c Diabetes
The long-term effects of necrosis on the pancreas can be severe, especially in type 3c diabetes.
As necrotic tissue builds up and damages pancreatic cells, it can lead to fibrosis, where the tissue becomes scarred and hardened.
This makes it even more difficult for the pancreas to function properly, as the scarred tissue replaces healthy, insulin-producing cells.
According to research in The Lancet Diabetes & Endocrinology, fibrosis as a result of necrosis severely limits the pancreas’s ability to produce insulin, leading to chronic high blood sugar levels.
The result is often a downward spiral where the pancreas becomes less and less capable of managing blood sugar levels, intensifying the effects of type 3c diabetes.
Real-Life Examples: How Necrosis Influences Pancreatic Functioning
Consider John, a 45-year-old who experienced acute pancreatitis due to gallstones.
The pancreatitis led to areas of necrosis in his pancreas, damaging his insulin-producing cells.
Post-recovery, John noticed he was constantly tired and thirsty, classic symptoms of diabetes.
Tests revealed that the necrosis had impaired his pancreas’s ability to produce insulin, and he was diagnosed with type 3c diabetes.
Another case is Sarah, a patient who underwent surgery on her pancreas after a traumatic accident.
During surgery, portions of her pancreas were removed, leading to necrotic tissue formation.
A few months later, Sarah began showing signs of high blood sugar.
Her doctors attributed this to type 3c diabetes, explaining that the necrosis in her pancreas was affecting her insulin levels.
Scientific Evidence on Necrosis and Type 3c Diabetes
Numerous studies have explored the link between necrosis and type 3c diabetes.
In Gastroenterology Research and Practice, researchers found that individuals with pancreatic necrosis were at a higher risk of developing type 3c diabetes due to the loss of insulin-producing cells.
The study emphasized that necrosis-induced inflammation plays a key role in the progression of type 3c diabetes.
Further evidence in The American Journal of Pathology confirms that necrosis disrupts normal pancreatic function by initiating a cascade of immune responses that ultimately result in cell death and tissue damage.
These findings help us understand why necrosis is such a critical factor in the onset and worsening of type 3c diabetes.
FAQs on Necrosis and Type 3c Diabetes
Q-1: How does pancreatic necrosis shrink both the enzyme-making and hormone-making parts of the gland?
A-1: Necrosis kills acinar cells (which make digestive enzymes) and can extend into islets (which release insulin, glucagon, and pancreatic polypeptide).
As dead tissue is cleared, it is replaced by scar and fat, shrinking the “working” pancreas. The result is a double hit: poorer digestion from enzyme loss and unstable glucose because fewer β-cells and α-cells remain to buffer post-meal highs and fasting lows.
Q-2: Why do glucose swings often worsen months after a necrotizing attack?
A-2: The injury doesn’t end when pain stops. Clean-up by immune cells and activation of pancreatic stellate cells continue for weeks, laying down collagen that stiffens ducts and compresses microvessels.
This slow scarring can choke off still-viable islets and acini, so people notice later changes—greasy stools, weight loss, and a shift from “borderline” sugars to overt Type 3c diabetes.
Q-3: What’s different about hormone balance when necrosis affects the pancreatic head versus the tail?
A-3: Head-dominant necrosis often reduces pancreatic polypeptide (PP), a hormone that normally restrains liver glucose output; fasting glucose may climb disproportionately.
Tail-dominant injury more often thins β-cell mass, blunting insulin peaks after meals. Either pattern can also weaken glucagon’s counter-regulation, making delayed hypoglycemia more likely after exercise or at night.
Q-4: How can walled-off necrosis or fluid collections keep digestion and glucose control unstable?
A-4: Collections that compress or kink ducts block enzyme flow, so fat and starch arrive in the intestine under-digested—dampening incretin signals that normally boost meal-time insulin.
Infected collections add systemic inflammation, which further impairs insulin action. After drainage or resolution, some people need less insulin or different mealtime dosing simply because digestion becomes more predictable again.
Q-5: What practical steps help when necrosis has already reduced pancreatic reserve?
A-5: Make digestion as efficient and steady as possible to reduce glucose chaos: take pancreatic enzymes with the first bite of meals and snacks, match dose to fat content, and consider acid suppression if enzymes underperform. Use smaller, protein-anchored meals to limit big swings.
Track patterns with a glucose meter/CGM—especially overnight—because weakened glucagon can hide delayed lows. Ask about fat-soluble vitamin testing (A, D, E, K) and bone health; repletion improves energy and training tolerance, which supports long-term glucose stability.
Conclusion
Necrosis has far-reaching implications for the pancreas, especially in individuals at risk of or diagnosed with type 3c diabetes.
When necrosis occurs, it not only damages pancreatic cells but also interferes with the pancreas’s ability to produce and regulate insulin, leading to the development of type 3c diabetes.
This tissue damage and inflammation create a challenging environment for the pancreas to recover or function normally, which can result in long-term blood sugar management issues.
References: