How Pancreatic Enzyme Insufficiency Affects Digestion in Type 3c Diabetes?
- admin
- November 10, 2024
- 5:47 pm
- No Comments
If digestion were a symphony, your pancreas would be the conductor, ensuring everything plays in harmony.
But what happens when the conductor steps down?
Enter pancreatic enzyme insufficiency (PEI), a common yet often overlooked complication of type 3c diabetes, also known as pancreatogenic diabetes.
In this article, BestDietarySupplementforDiabetics research team shall explore how PEI disrupts digestion, the ripple effects it has on overall health, and the science behind it.
Expect witty insights, real-life examples, and a dive into the interconnected worlds of enzymes, digestion, and diabetes.
By the end, you would understand why managing PEI is essential for people living with type 3c diabetes.
What is Included in this Article?
- What Is Pancreatic Enzyme Insufficiency?
- The Role of the Pancreas in Digestion
- How Pancreatic Enzyme Insufficiency Develops in Type 3c Diabetes
- The Digestive Chaos: Malabsorption Explained
- Real-Life Example: Lucy’s Struggle with PEI and Type 3c Diabetes
- Scientific Studies Linking PEI and Type 3c Diabetes
- FAQS on Diabetes and Pancreatic Enzyme Deficiency in Type 3C Diabetes
- The Long-Term Impact of Poor Digestion in Type 3c Diabetes
- Conclusion: The Need to Address PEI in Type 3c Diabetes
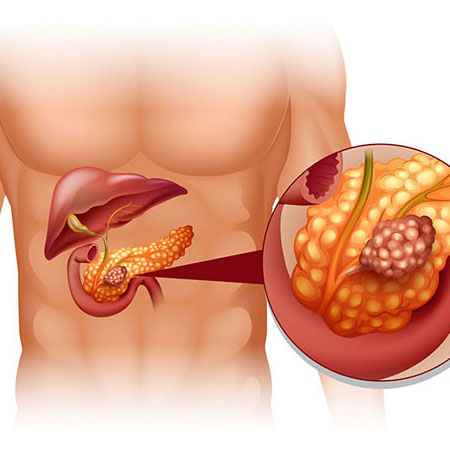
What Is Pancreatic Enzyme Insufficiency?
Pancreatic enzyme insufficiency occurs when the pancreas fails to produce enough enzymes to properly digest food.
These enzymes—amylase, lipase, and protease—are critical for breaking down carbohydrates, fats, and proteins.
Without them, food remains partially digested, leading to malabsorption and a cascade of gastrointestinal symptoms like bloating, diarrhea, and unintentional weight loss.
In type 3c diabetes, PEI is particularly common because the pancreas is already under siege.
Chronic pancreatitis, pancreatic surgery, or tumors often damage the organ’s ability to produce these enzymes.
Unfortunately, this condition does not just affect digestion—it impacts overall health.
The Role of the Pancreas in Digestion
Your pancreas is like the overachiever of your body’s organs—a multitasking marvel that somehow manages to juggle blood sugar regulation and digestion without breaking a sweat.
While its insulin-production skills often hog the spotlight, its role in digestion is just as important.
Think of your pancreas as the manager of a top-tier restaurant kitchen, overseeing the enzymes that make nutrient absorption possible.
Here is the team:
- Amylase: The pastry chef, breaking down carbohydrates into simple sugars that give you quick energy.
- Lipase: The sous chef, handling fats and converting them into fatty acids and glycerol for easy absorption.
- Protease: The grill master, slicing and dicing proteins into amino acids for muscle repair and cellular upkeep.
When your pancreas is not pulling its weight—thanks to chronic conditions like pancreatitis or type 3c diabetes—this culinary dream team falls apart.
Production slows, digestion becomes inefficient, and your body misses out on the vital nutrients it needs.
It is quite similar to running a restaurant during a staff shortage: orders (nutrients) pile up, dishes (digestion) take forever, and customers (your body) leave unsatisfied.
A struggling pancreas means your digestive system is constantly playing catch-up, leading to issues like bloating, malnutrition, and fatigue.
Let us face it: your body deserves a five-star kitchen, and the pancreas is the head chef it can’t do without.
How Pancreatic Enzyme Insufficiency Develops in Type 3c Diabetes?
Type 3c diabetes is distinct from type 1 and type 2 diabetes in both cause and mechanism.
Unlike type 2, which arises from insulin resistance, or type 1, which results from autoimmune destruction of insulin-producing beta cells, type 3c diabetes stems from direct damage to the pancreas.
This damage can occur due to conditions such as chronic pancreatitis, pancreatic cancer, or surgical interventions that impair the pancreas’s ability to function.
The pancreas has two critical roles: producing hormones (endocrine function) and digestive enzymes (exocrine function).
When the pancreas is damaged, both functions are compromised, though the impact on digestion often goes unnoticed at first. Digestive enzyme production takes a backseat as the pancreas prioritizes survival over efficiency.
This leads to pancreatic enzyme insufficiency (PEI), a condition where the pancreas cannot produce enough enzymes to break down food properly.
Over time, PEI adds a new layer of complexity to managing type 3c diabetes. Poor digestion exacerbates malnutrition, weight loss, and energy deficiencies while complicating blood sugar control.
Understanding this interconnected relationship between pancreatic damage, enzyme insufficiency, and type 3c diabetes is crucial for developing comprehensive management strategies that address not just blood sugar levels, but overall digestive health and nutrition.
The Digestive Chaos: Malabsorption Explained
Malabsorption takes center stage in the digestive challenges caused by pancreatic enzyme insufficiency (PEI). When the pancreas struggles to produce its vital enzymes, digestion falters, and nutrient absorption suffers.
Here is a closer look at the ripple effects:
1. Carbohydrate Malabsorption:
Without sufficient amylase, carbohydrates cannot be broken down into simple sugars.
Instead of providing energy, undigested carbs ferment in the gut, leading to excessive gas, bloating, and discomfort.
Over time, this deprives the body of a primary energy source.
2. Fat Malabsorption (Steatorrhea):
Lipase deficiency means dietary fats remain undigested, resulting in greasy, foul-smelling stools—a hallmark of fat malabsorption.
The body also struggles to absorb fat-soluble vitamins (A, D, E, and K), which are essential for vision, bone health, immunity, and skin integrity.
This deficiency can cause long-term complications like osteoporosis and impaired immune responses.
3. Protein Malabsorption:
Protease, responsible for breaking down proteins into amino acids, is also affected.
Without it, protein absorption is compromised, leading to muscle wasting, fatigue, and reduced ability to repair tissues or fight infections.
These cumulative effects of malabsorption lead to malnutrition, unintentional weight loss, and a weakened body.
The result is not just physical discomfort but a significant impact on overall health, making PEI a critical factor in conditions like type 3c diabetes that require immediate attention.
Real-Life Example: Lucy’s Struggle with PEI and Type 3c Diabetes
Lucy, a 48-year-old teacher, was diagnosed with type 3c diabetes after years of battling chronic pancreatitis.
She noticed symptoms like bloating, diarrhea, and unintentional weight loss but chalked them up to stress.
Her doctor suspected pancreatic enzyme insufficiency and prescribed enzyme replacement therapy.
Within weeks, Lucy’s symptoms improved. She regained energy, her digestive discomfort eased, and she began maintaining a healthy weight.
Lucy’s story highlights the often-overlooked connection between PEI and type 3c diabetes.
Addressing digestive health transformed her quality of life, showing how critical it is to manage PEI alongside diabetes.
Scientific Studies Linking PEI and Type 3c Diabetes
The relationship between pancreatic enzyme insufficiency (PEI) and type 3c diabetes is well-documented in scientific research, shedding light on the complex interplay between digestive health and blood sugar management.
1. “Exocrine Pancreatic Insufficiency in Diabetes Mellitus” (Diabetes Care, 2018)
This pivotal study revealed that up to 50% of individuals with type 3c diabetes experience PEI.
The condition results in significant malabsorption of nutrients, leading to symptoms like unintentional weight loss, steatorrhea (fatty stools), and bloating.
These digestive issues compound the challenges of managing diabetes effectively, highlighting the need for integrated care.
2. “Nutritional Deficiencies in Pancreatogenic Diabetes” (Clinical Nutrition, 2020)
This research emphasized the link between PEI and deficiencies in fat-soluble vitamins (A, D, E, and K).
Such deficiencies can lead to complications like osteoporosis, weakened immunity, and poor vision, further deteriorating health in patients with type 3c diabetes.
Addressing malabsorption is critical to improving nutrient status and preventing long-term complications.
3. “Impact of Digestive Dysfunction on Glycemic Control” (Pancreatology, 2019)
This study explored how digestive dysfunction caused by PEI destabilizes blood sugar levels, complicating diabetes management.
Poor nutrient absorption disrupts the balance of macronutrients, leading to erratic glucose levels and making insulin or medication adjustments more challenging.
These findings collectively highlight the necessity of recognizing and treating PEI as a core component of type 3c diabetes care to improve both digestive health and glycemic control.
FAQS on Diabetes and Pancreatic Enzyme Deficiency in Type 3C Diabetes
Q-1: How does pancreatic enzyme insufficiency change the timing of nutrient absorption—and why does that matter for glucose in Type 3c diabetes?
A-1: When the pancreas does not supply enough enzymes and bicarbonate, food reaches the small intestine but is not fully broken down. Carbs, fats, and proteins move along only partially digested (pancreatic enzyme insufficiency adversely affects your digestion), so absorption happens later and less predictably.
Instead of a typical early post-meal rise, glucose may spike an hour or two afterward—or barely rise at all—making dosing and meal planning tricky. Effective pancreatic enzyme replacement therapy (PERT) can restore more “on-time” digestion, improving symptom control and making post-meal glucose patterns easier to interpret.
Q-2: Can enzyme insufficiency blunt gut-hormone (incretin) signals that normally help control post-meal glucose?
A-2: Yes. Fat digestion products and bile acids help trigger gut hormones like GLP-1 that coordinate insulin release and slow gastric emptying. If fats aren’t broken down well, those signals are weaker.
In Type 3c diabetes—where exocrine failure is common—dampened incretin responses can worsen post-meal control. By improving intraluminal digestion, PERT can support a more normal cascade of gut signals, which may translate to steadier glucose after meals, even if insulin requirements still need fine-tuning.
Q-3: Why do some people still have steatorrhea or bloating on enzymes—and how can that disrupt nutrition in Type 3c diabetes?
A-3: Persistent symptoms often reflect factors beyond enzyme dose. Small intestinal bacterial overgrowth or abdominal trauma can deconjugate bile acids, keeping fat malabsorption going despite PERT. Acidic duodenal pH can inactivate enzymes before they work.
Irregular timing—taking enzymes after the meal or using too few capsules—also undermines results. The fallout is gas, cramps, weight loss, and poor uptake of calories and fat-soluble vitamins. Solutions include optimizing timing (first bite and mid-meal), adjusting dose based on fat content, adding acid suppression when appropriate, and treating bacterial overgrowth.
Q-4: Which nutrient deficits are most tied to enzyme failure—and what should people with Type 3c watch for when starting PERT?
A-4: Fat-soluble vitamins A, D, E, and K are most vulnerable; low vitamin D is particularly common and can affect bone and muscle health. Starting PERT often improves stools, appetite, and weight stability.
One caveat: better digestion increases carbohydrate availability, so some people see higher or earlier post-meal glucose and need to adjust insulin or meal composition. A practical checklist: baseline vitamin levels (especially D and E), enzyme dosing with every meal and snack, consistent timing, and closer glucose monitoring during the first few weeks of effective therapy.
The Long-Term Impact of Poor Digestion in Type 3c Diabetes
If left untreated, pancreatic enzyme insufficiency (PEI) can lead to a cascade of severe complications, particularly in individuals with type 3c diabetes.
The inability to properly digest and absorb nutrients affects multiple systems in the body, compounding health challenges over time.
- Malnutrition: Chronic malabsorption deprives the body of essential nutrients, leading to deficiencies in vitamins, minerals, and macronutrients. This weakens the immune system, making it harder for the body to fight infections and recover from illnesses.
- Weight Loss and Muscle Wasting: The inability to absorb calories exacerbates unintentional weight loss. Over time, this leads to muscle wasting, reduced physical strength, and overall frailty, which can impact daily activities and quality of life.
- Bone Health Issues: Fat malabsorption prevents the absorption of fat-soluble vitamins like vitamin D, which is critical for calcium metabolism. This increases the risk of osteoporosis and fractures, posing a significant threat to mobility and long-term bone health.
- Diabetes Management Challenges: Malabsorption disrupts nutrient availability, complicating blood sugar regulation. Erratic glucose levels make insulin or medication adjustments more difficult, creating a vicious cycle of poor health outcomes.
These long-term effects underscore the urgent need for proactive management of digestive health in type 3c diabetes.
Addressing PEI through early diagnosis and targeted interventions can prevent these complications, improving both digestive function and overall well-being.
Proper care ensures that PEI doesn’t silently worsen the challenges of managing type 3c diabetes.
The Need to Address PEI in Type 3c Diabetes
Pancreatic enzyme insufficiency is a silent but powerful contributor to the challenges faced by people with type 3c diabetes.
Beyond regulating blood sugar, the pancreas plays a vital role in digestion.
When enzyme production falters, the ripple effects impact everything from nutrient absorption to overall well-being.
You also need to learn that gallstones cause inflammation in the pancreas, which in turn complicates into type 3c diabetes.
Understanding how PEI affects digestion is key to improving quality of life for those living with type 3c diabetes.
Addressing these issues through awareness, diagnosis, and targeted treatments can transform health outcomes, ensuring that digestion is not an overlooked part of diabetes management.
References: