How Pancreatic Fibrosis Impacts Insulin Production?
- admin
- November 2, 2024
- 7:57 pm
- No Comments
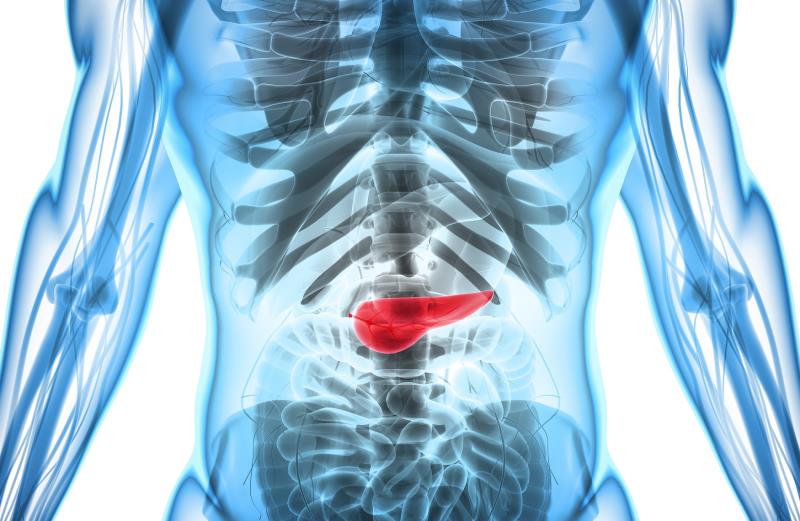
The pancreas are often overlooked but endlessly hardworking.
This little organ plays a pivotal role in keeping your blood sugar in check.
When it is in good shape, the pancreas quietly churns out insulin, ensuring that your body’s cells get the energy they need.
But what happens when things go south—specifically, when pancreatic fibrosis shows up?
Spoiler alert: its i not good news.
Pancreatic fibrosis can be a silent saboteur, messing with your insulin production and leaving you vulnerable to all sorts of metabolic mayhem.
Today, we are diving into how pancreatic fibrosis affects insulin production, breaking down the science in a way that would not make you want to doze off.
From the nitty-gritty cellular disruptions to real-world stories, we have got a lot to unpack.
Article Index:
- What is Pancreatic Fibrosis?
- How the Pancreas Normally Produces Insulin
- The Fibrotic Interference: How Fibrosis Disrupts Insulin Secretion
- Real-Life Example: Meet Alex, the Athlete Turned Diabetic
- The Inflammatory Connection and Why It Matters
- The Vicious Cycle: How Fibrosis Worsens Over Time
- Conclusion: Understanding the Impact Without Offering a Fix
What is Pancreatic Fibrosis?
Let us start with the basics.
Pancreatic fibrosis occurs when healthy pancreatic tissue gets replaced by scar tissue.
This scarring can be the result of chronic inflammation, injuries, or conditions like pancreatitis.
Think of it like replacing a sponge with a rock: the pancreas becomes stiff and less functional, which is a major problem considering it is supposed to be soft and squishy to work efficiently.
According to The Journal of Clinical Investigation, pancreatic fibrosis not only hampers the overall structure of the pancreas but also interferes with its essential duties, like enzyme and hormone production.
How the Pancreas Normally Produces Insulin?
Before we get to the fibrotic drama, let us appreciate the pancreas in its full glory.
The pancreas is split into two main functions: the exocrine (enzyme-producing) and endocrine (hormone-producing) systems.
Insulin, our star hormone here, is produced by beta cells in clusters known as the islets of Langerhans.
These cells constantly monitor your blood sugar levels and release insulin as needed to help regulate glucose.
Endocrine Reviews notes that a healthy pancreas can adjust insulin output almost instantly, keeping your blood sugar levels stable.
It is like having a thermostat that adjusts the temperature the moment it starts to get too hot or too cold.
But with pancreatic fibrosis in the picture, this smooth operation becomes a hot mess.
The Fibrotic Interference: How Fibrosis Disrupts Insulin Secretion?
So, how does fibrosis throw a wrench into the pancreas’s insulin-making machinery?
When scar tissue invades the pancreas, it physically displaces and compresses the islets of Langerhans.
This reduces the number of functioning beta cells and compromises the pancreas’s ability to sense and respond to blood glucose levels.
A study from Diabetes Care found that individuals with significant pancreatic fibrosis had notably impaired insulin secretion.
In simpler terms, it is like having fewer workers on a factory line: production slows down, and quality control goes out the window.
The damaged beta cells cannot keep up with insulin demands, leading to hyperglycemia (high blood sugar levels).
Meet Alex, the Athlete Turned Diabetic
To put a face to this condition, let’s talk about Alex.
Alex was a high school track star who never thought twice about his pancreas—until he started experiencing unexplained fatigue and thirst.
A visit to the doctor and some tests later, he found out that chronic pancreatic inflammation had led to fibrosis, which was severely affecting his insulin production.
His athletic performance plummeted, and managing his blood sugar became a daily struggle.
He had to learn the art of managing his blood sugar levels using natural methods.
Alex’s story is a stark reminder that pancreatic fibrosis is not just a condition for the old and unfit; it can impact anyone, disrupting their ability to live a normal, healthy life.
The Inflammatory Connection and Why It Matters?
Here is where things get even more complicated.
Chronic inflammation plays a starring role in pancreatic fibrosis.
Conditions like chronic pancreatitis or autoimmune diseases keep the pancreas in a constant state of defense.
The longer the inflammation persists, the more scar tissue forms, worsening the fibrosis.
According to Nature Reviews Gastroenterology & Hepatology, ongoing inflammation leads to a self-perpetuating cycle: inflammation causes fibrosis, which leads to more inflammation, and so on.
This inflammatory environment not only damages beta cells but also makes them less effective at producing insulin.
The pancreas is essentially stuck in a bad feedback loop, and insulin production takes a serious hit.
The Vicious Cycle: How Fibrosis Worsens Over Time?
Fibrosis does not just hit pause once it starts; it is a progressive condition.
Over time, more and more pancreatic tissue becomes scarred, reducing the organ’s functionality.
This creates a vicious cycle: as insulin production declines, blood sugar levels spike, leading to further complications and metabolic stress.
A study in Pancreas Journal illustrates this cycle well, showing that even a slight increase in fibrosis can lead to exponential declines in insulin production.
It is a downward spiral that is hard to break, emphasizing the need for early detection and management.
Unfortunately, the damage is often irreversible by the time significant symptoms appear.
Understanding the Impact Without Offering a Fix
So, how does pancreatic fibrosis impact insulin production?
In short, it wreaks havoc.
The fibrosis displaces and damages the insulin-producing beta cells, while chronic inflammation exacerbates the situation.
Over time, this scar tissue makes it increasingly difficult for the pancreas to produce and secrete insulin, leading to a cascade of metabolic problems.
Understanding this connection can be a game-changer in recognizing early symptoms and getting a proper diagnosis.
While this article does not offer solutions, it should give you a clearer picture of why pancreatic health is so crucial and how fibrosis can derail one of your body’s most vital functions.
References: