How Pancreatitis Leads to Type 2 Diabetes?
- admin
- October 30, 2024
- 3:53 pm
- No Comments
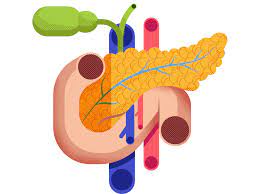
If you have ever thought of the pancreas as just another digestive organ, it is time to give it a second look.
This small, essential organ does a lot more than process enzymes for digestion—it is also crucial for blood sugar regulation.
Unfortunately, when the pancreas is damaged due to inflammation, as seen in pancreatitis, it can throw off blood sugar levels and, over time, lead to type 2 diabetes.
In this article, we shall explore how pancreatitis and type 2 diabetes are linked, the role of the pancreas in blood sugar control, and why inflammation can lead to diabetes development.
Article Index:
- What Is Pancreatitis and Why Does It Matter?
- How the Pancreas Regulates Blood Sugar
- The Impact of Pancreatitis on Insulin Production
- Why Inflammation in the Pancreas Can Trigger Type 2 Diabetes
- Real-Life Examples of Pancreatitis Leading to Diabetes
- Conclusion: Steps to Protect Your Pancreas and Prevent Diabetes
What Is Pancreatitis and Why Does It Matter?
Pancreatitis is the inflammation of the pancreas, often caused by excessive alcohol use, gallstones, or genetic predisposition.
The pancreas is responsible for releasing enzymes to help digest food and hormones, primarily insulin, to manage blood sugar levels.
When the pancreas becomes inflamed, these functions can become compromised.
According to the American Diabetes Association, chronic inflammation in the pancreas can damage the cells responsible for insulin production, leading to blood sugar imbalances and potentially type 2 diabetes.
Pancreatitis can be acute, where symptoms come on suddenly, or chronic, where inflammation recurs over time and leads to permanent damage.
Both types of pancreatitis can contribute to the risk of type 2 diabetes, but chronic pancreatitis is especially impactful because it leads to lasting damage to insulin-producing cells.
How the Pancreas Regulates Blood Sugar?
The pancreas plays a crucial role in blood sugar regulation by releasing insulin, a hormone that allows cells to absorb glucose for energy.
When blood sugar levels are high, insulin production ramps up; when blood sugar is low, insulin release slows down.
This delicate balance is essential for keeping blood sugar levels within a healthy range.
In type 2 diabetes, this regulatory mechanism becomes impaired.
The pancreas either cannot produce enough insulin, or the body’s cells become resistant to it, leading to high blood sugar levels.
In cases where pancreatitis has damaged insulin-producing cells (known as beta cells), the pancreas becomes less effective at managing blood sugar, contributing to diabetes development.
The Impact of Pancreatitis on Insulin Production?
When the pancreas is inflamed, as seen in pancreatitis, the inflammation affects the pancreas’s ability to produce insulin effectively.
Chronic pancreatitis leads to long-term damage to beta cells, which are the cells responsible for insulin production.
Studies, such as one published in Diabetes Care, have shown that people with chronic pancreatitis are at a significantly higher risk of developing type 2 diabetes compared to the general population.
The pancreas is like a machine that regulates blood sugar, but when it is damaged by chronic inflammation, it cannot maintain this balance.
In The Journal of Clinical Endocrinology & Metabolism, researchers explain how the progressive destruction of beta cells in chronic pancreatitis patients leaves them with reduced insulin production, often resulting in blood sugar levels that are more challenging to manage.
As a result, these patients frequently develop what is known as pancreatogenic or “type 3c diabetes,” which shares characteristics with type 2 diabetes but is specifically caused by pancreatic disease.
Why Inflammation in the Pancreas Can Trigger Type 2 Diabetes?
Inflammation has long been recognized as a key driver of many chronic diseases, including diabetes.
When the pancreas is inflamed, the inflammatory process damages insulin-producing cells, leading to scar tissue formation.
This scarring or fibrosis makes it difficult for the pancreas to produce insulin effectively.
According to research from The Lancet Diabetes & Endocrinology, inflammation within the pancreas not only affects insulin production but can also impair how effectively insulin works, creating a “double whammy” effect that drives blood sugar levels higher.
This combination of decreased insulin production and reduced insulin effectiveness is a recipe for type 2 diabetes development.
In addition, as inflammation persists, the pancreas undergoes a process called fibrosis, where healthy tissue is replaced with scar tissue.
Over time, this fibrosis can spread throughout the pancreas, permanently impairing its ability to regulate blood sugar.
Real-Life Examples of Pancreatitis Leading to Diabetes
To understand how pancreatitis can impact daily life and potentially lead to diabetes, let’s look at a real-life scenario:
Example: Rachel’s Story:
Rachel, a 50-year-old with a history of heavy drinking, developed chronic pancreatitis after years of inflammation in her pancreas.
Although she initially managed her condition with dietary changes, her pancreas began to lose its ability to produce insulin.
Rachel’s blood sugar levels became harder to control, and she was ultimately diagnosed with type 2 diabetes as a result of her chronic pancreatitis.
Rachel’s experience underscores the critical connection between long-term inflammation in the pancreas and the development of diabetes.
Here is John’s Experience:
John, a middle-aged man who struggled with gallstone-induced pancreatitis, found himself experiencing fluctuating blood sugar levels after a few acute episodes.
Despite managing his gallstones, his pancreas had already suffered damage.
With time, his insulin production declined, eventually leading to a type 2 diabetes diagnosis.
John’s case highlights how even episodic inflammation can contribute to long-term pancreas damage and set the stage for diabetes.
Steps to Protect Your Pancreas and Prevent Diabetes
While pancreatitis is a serious condition that can increase the risk of type 2 diabetes, there are preventive steps you can take to support pancreas health and reduce your diabetes risk:
-
Adopt a Pancreas-Friendly Diet: Focus on low-fat, high-fiber foods to support your pancreas. A diet rich in fruits, vegetables, and lean proteins can help reduce inflammation and ease digestive strain on the pancreas.
-
Limit Alcohol Intake: Alcohol is a major contributor to pancreatitis, so limiting or eliminating alcohol can help protect the pancreas. According to The American Journal of Gastroenterology, abstaining from alcohol is one of the most effective ways to prevent pancreatitis progression.
-
Maintain a Healthy Weight: Carrying excess weight can strain the pancreas. Studies published in The British Medical Journal show that a healthy weight can support pancreas function and reduce the risk of diabetes.
-
Monitor Blood Sugar Levels: For individuals with a history of pancreatitis, regular blood sugar monitoring can help detect early signs of diabetes. Early intervention can help manage blood sugar levels naturally and delay the onset of diabetes.
Pancreatitis and type 2 diabetes are closely linked, with chronic inflammation in the pancreas creating a cascade of changes that impair insulin production and increase the risk of diabetes.
By understanding the relationship between pancreatitis and blood sugar regulation, we can take proactive steps to protect pancreas health and potentially prevent diabetes development.
References: