How Partial Pancreatectomy Triggers Type 3c Diabetes?
- admin
- November 5, 2024
- 11:07 am
- No Comments
Well, the pancreas.
It might not be the most glamorous organ—it is no heart or brain—but boy, does it play a starring role when it comes to digestion and blood sugar regulation.
Now, imagine having to bid farewell to part of this hardworking organ through a surgical procedure called partial pancreatectomy.
What happens next?
Unfortunately, losing a chunk of your pancreas can be more than just an inconvenience.
It can lead to type 3c diabetes, a condition that does not get the limelight as much as its type 1 and type 2 siblings but is just as significant.
In this article, I will dissect (pun intended) how and why this happens, looking into the biology, the mechanics, and some real-life stories along the way.
Points Covered in this Article:
- What Is a Partial Pancreatectomy?
- How the Pancreas Regulates Blood Sugar
- The Connection Between Pancreatectomy and Type 3c Diabetes
- Hormonal Changes After Partial Pancreatectomy
- Real-Life Example: Lisa’s Journey Post-Surgery
- FAQs on Partial Pancreatectomy and Type 3c Diabetes
- The Role of the Spleen: Why Partial Pancreatectomy and Splenectomy Complicate Matters
- Complications Beyond Blood Sugar: Other Impacts of Partial Pancreatectomy
- Recovery and Management: Life After Partial Pancreatectomy
- Conclusion: The Unfortunate Consequences We Need to Understand
What Is a Partial Pancreatectomy?
Let’s kick things off with some basics.
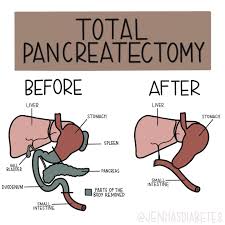
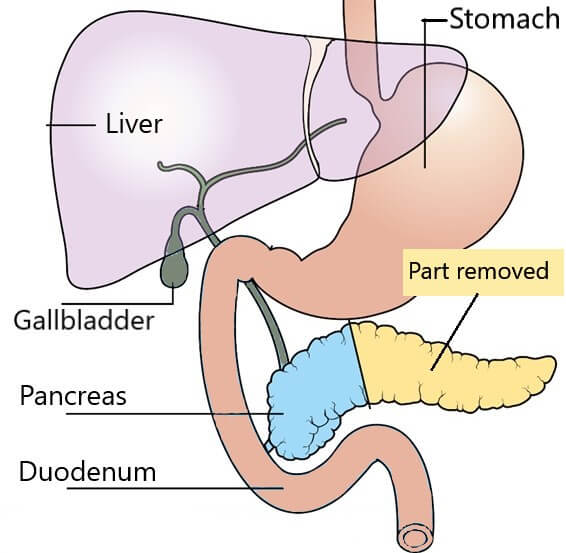
A partial pancreatectomy is a surgical procedure where a portion of the pancreas is removed.
Why would anyone undergo this, you ask?
It is usually performed to treat conditions like pancreatic tumors, chronic pancreatitis, or cysts.
The pancreas is split into three parts: the head, body, and tail.
Depending on the location of the issue, different parts may be removed.
Sometimes, this surgery also involves taking out the spleen, a procedure called partial pancreatectomy and splenectomy.
Now, the pancreas is not just sitting around idly.
It has two main jobs: producing digestive enzymes and regulating blood sugar.
You can probably guess where this is going—messing with the pancreas is bound to cause some problems.
How the Pancreas Regulates Blood Sugar?
Our star organ, the pancreas, has a secret weapon: islet cells.
These clusters of cells produce hormones like insulin and glucagon, which are crucial for keeping our blood sugar in check.
Insulin helps lower blood sugar by facilitating glucose absorption into cells, while glucagon raises blood sugar when it dips too low.
Now, imagine taking a slice out of the pancreas.
When these hormone-producing cells are reduced, the body’s ability to regulate blood sugar takes a nosedive.
The Journal of Clinical Endocrinology & Metabolism highlights that even a small reduction in pancreatic tissue can significantly disrupt insulin production.
The Connection Between Pancreatectomy and Type 3c Diabetes
Type 3c diabetes, also known as pancreatogenic diabetes, is a form of diabetes caused by the loss of pancreatic function.
It is different from type 1 and type 2 diabetes because the root problem is not autoimmune destruction or insulin resistance—it is a lack of insulin due to pancreatic damage.
According to Diabetes Care, up to 10% of all diabetes cases could actually be type 3c, but it often goes misdiagnosed.
Here is the crux: when a portion of the pancreas is removed, the balance of insulin and other hormones gets disrupted.
This imbalance makes it hard for the body to manage blood sugar levels, and voila, you have type 3c diabetes.
Hormonal Changes After Partial Pancreatectomy
The pancreas is not just a one-trick pony.
Aside from insulin, it produces other hormones that aid digestion and metabolism.
When part of the pancreas is removed, these hormones can’t do their jobs properly.
Reduced insulin means higher blood sugar levels, while a lack of digestive enzymes leads to malabsorption of nutrients.
Studies published in Pancreatology show that patients often experience drastic hormonal shifts, making diabetes management incredibly tricky.
Unlike type 2 diabetes, where lifestyle changes can help manage the condition, type 3c diabetes often requires insulin therapy from the get-go.
Real-Life Example: Lisa’s Journey Post-Surgery
Meet Lisa, a 52-year-old teacher who had a partial pancreatectomy to remove a benign tumor.
Before the surgery, she had never had any issues with her blood sugar.
But within months of the procedure, she found herself feeling fatigued and thirsty all the time.
A visit to the doctor confirmed her fears: she had developed type 3c diabetes.
“I had no idea this could happen,” Lisa shared. “I thought I would just have to recover from the surgery and that would be it.
Now, I am learning to manage my blood sugar, and it is a whole new challenge.”
Lisa’s experience is not unique.
Many people are not warned about the risk of diabetes following a partial pancreas removal, which makes coping even more difficult.
The Role of the Spleen: Why Partial Pancreatectomy and Splenectomy Complicate Matters?
Sometimes, surgeons have to remove the spleen along with part of the pancreas, especially if they are dealing with tumors or severe trauma.
The spleen plays a role in immunity and filtering blood, and removing it can make diabetes management even more complicated.
Without a spleen, the body is more prone to infections, which can further destabilize blood sugar levels.
According to The British Journal of Surgery, patients who undergo both partial pancreatectomy and splenectomy face a higher risk of developing diabetes and other metabolic complications.
It is a double whammy that makes recovery even more complex.
Complications Beyond Blood Sugar: Other Impacts of Partial Pancreatectomy
The complications of partial pancreatectomy do not stop at diabetes.
Patients may experience malnutrition, digestive issues, and chronic fatigue.
The loss of digestive enzymes means that even a well-balanced diet may not be fully absorbed.
Gastroenterology Research highlights the prevalence of nutrient deficiencies in patients post-surgery.
Imagine eating a healthy meal but only absorbing half of the nutrients.
That is the reality for many who have had this surgery, and it adds an extra layer of difficulty to managing diabetes and overall health.
Recovery and Management: Life After Partial Pancreatectomy
Recovery from a partial pancreatectomy is no walk in the park.
Patients have to adjust to a new way of living, which often includes enzyme supplements and a strict diet.
Partial pancreatectomy recovery can be long and arduous, with complications like digestive discomfort and fluctuating blood sugar levels.
Regular follow-ups with endocrinologists and dietitians are crucial.
Managing type 3c diabetes often requires a team approach, and many patients have to learn how to use insulin, monitor their blood sugar levels, and adapt to new dietary restrictions.
FAQs on Partial Pancreatectomy and Type 3c Diabetes
Q-1: Why does the location of resection (head vs. tail) change the diabetes pattern after surgery?
A-1: Head resections often reduce pancreatic polypeptide (PP), a hormone that normally reins in the liver’s glucose output. With less PP, fasting glucose can climb because the liver behaves “overactive.” Tail (distal) resections remove more of the islet-dense region that produces insulin, so meal-time spikes are more prominent. Either surgery can also blunt glucagon responses, widening swings between highs and lows.
Q-2: Why is post-pancreatectomy diabetes often “brittle,” with surprising lows despite clear hyperglycemia?
A-2: It’s not just less insulin—counter-regulation is impaired too. Many people lose a reliable glucagon response after partial pancreatectomy, so the usual liver “rescue” during exercise, overnight, or after a slightly aggressive insulin dose is muted. That’s why cautious titration, bedtime checks, and familiarity with late-onset hypoglycemia are emphasized even when average glucose runs high.
Q-3: How do exocrine changes after surgery alter incretin biology—and insulin needs?
A-3: Resection commonly leads to exocrine pancreatic insufficiency. Poor digestion of fats and starch changes what reaches the lower gut, dulling incretin signals that normally boost meal-time insulin. When pancreatic enzyme replacement is taken with the first bite and matched to meal fat, digestion becomes more predictable, incretin support improves, and mealtime insulin timing or dose often needs recalibration.
Q-4: How common is new-onset diabetes after distal pancreatectomy, and who’s at highest risk?
A-4: Risk varies with why and how much tissue is removed. Across mixed surgical indications, roughly a quarter to a third of patients develop new-onset diabetes after distal pancreatectomy; the risk is higher with larger resections, underlying chronic pancreatitis, and in some cohorts, male sex. Many who develop diabetes after distal resection ultimately require insulin, reflecting the reduced β-cell reserve.
Q-5: Are there targeted strategies to counter the specific hormone defects after partial pancreatectomy?
A-5: Match therapy to the physiology.
- Hepatic drive (PP loss): Focus on fasting control and hepatic glucose output—small changes to overnight regimens and morning routines often help.
- Incretin support: Optimize enzyme replacement and meal structure (protein-anchored, moderate fat, consistent timing) to stabilize post-meal insulin needs.
- Counter-regulation: Expect weaker glucagon. Favor conservative insulin titration, use CGM with alerts, and time vigorous exercise away from peak insulin action. Education on late and nocturnal lows is as important as hitting A1C targets.
Takeaway: Partial pancreatectomy creates distinct endocrine “footprints” depending on what’s removed. Add exocrine changes and weaker counter-regulation, and you get the characteristic Type 3c pattern—manageable with digestion-first strategies, tailored insulin, and vigilant safety planning.
The Unfortunate Consequences We Need to Understand
In the world of diabetes, type 3c is often the underdog, but for those who have undergone partial pancreas removal, it is a very real and challenging condition.
The relationship between partial pancreatectomy and type 3c diabetes is complex, affecting everything from hormone production to nutrient absorption.
Understanding this link is crucial, not just for patients but also for healthcare providers.
References: