How PCOS Affects Insulin Resistance?
- admin
- October 27, 2024
- 7:33 am
- No Comments

Polycystic Ovary Syndrome (PCOS) and insulin resistance are two conditions often found in a complicated and intertwined relationship.
If you have ever wondered why managing weight or blood sugar seems particularly challenging with PCOS, insulin resistance might be the culprit.
Today, we are diving into the science behind it: how PCOS affects insulin resistance, what you can do about it, and why it is crucial to understand this connection for better health management.
“How PCOS Affects Insulin Resistance” Article Index
- Introduction to PCOS and Insulin Resistance
- The Link Between Hormones, Insulin, and PCOS
- Real-Life Impact: Examples of PCOS and Insulin Resistance
- Symptoms of Insulin Resistance in PCOS
- Strategies to Manage Insulin Resistance in PCOS
- Conclusion: Breaking the Cycle
Introduction to PCOS and Insulin Resistance
Polycystic Ovary Syndrome (PCOS) is a complex hormonal condition that affects an estimated 5% to 18% of women of reproductive age worldwide.
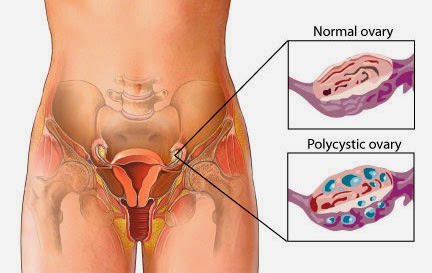
Though it is most often associated with irregular periods, ovarian cysts, and acne, one of the most critical and often overlooked aspects of PCOS is insulin resistance.
In fact, between 50% to 70% of women with PCOS experience insulin resistance—even those who are not overweight. This means their bodies do not respond to insulin as efficiently as they should, causing the pancreas to produce more insulin to compensate.
Over time, this can trigger a host of metabolic problems, including weight gain, type 2 diabetes, and worsening hormonal imbalances.
The relationship between insulin resistance and PCOS is bidirectional. On one hand, insulin resistance can lead to increased levels of androgens (male hormones), which worsen PCOS symptoms like hirsutism and acne.
On the other hand, the hormonal imbalances associated with PCOS can make insulin resistance even more pronounced. It becomes a vicious cycle if not managed early.
Recent scientific studies have explored this connection in greater depth, identifying possible biomarkers like growth differentiation factor 15 (GDF15) that may help monitor the severity of insulin resistance in PCOS.
Some researchers are also examining genetic and molecular mechanisms to better understand why insulin resistance and PCOS often go hand in hand.
On a positive note, certain treatments like myo-inositol supplementation and newer GLP-1 receptor agonist medications are showing promise in improving insulin sensitivity and hormonal balance.
These approaches may also support weight management and improve menstrual regularity in many women.
Understanding this connection is key—not just for treating PCOS, but also for preventing long-term health risks associated with insulin resistance. Early intervention can make a world of difference.
The Link Between Hormones, Insulin, and PCOS
When we talk about insulin resistance, it means the body’s cells do not respond properly to insulin, which is essential for regulating blood sugar levels.
To compensate, the pancreas produces even more insulin, resulting in “hyperinsulinemia in PCOS.”
Elevated insulin levels stimulate the ovaries to produce more androgens (male hormones), leading to symptoms like irregular periods, excessive hair growth, and weight gain (Imaware, 2023).
Additionally, research highlights that high insulin levels in PCOS disrupt fat metabolism, leading to abdominal weight gain—a common issue in women with PCOS.
This accumulation of abdominal fat further fuels insulin resistance, creating a vicious cycle that is challenging to break (Journal of Ovarian Research, 2020).
Real-Life Impact: Examples of PCOS and Insulin Resistance
Take, for example, Lisa, a 32-year-old diagnosed with PCOS and struggling with weight gain despite her efforts to maintain a balanced diet.
Her doctor found elevated “fasting insulin levels in PCOS,” indicating insulin resistance.
Even though she wasn’t diabetic, her body required more insulin to manage blood sugar, contributing to her difficulty in losing weight.
Another case is Lisa, who had been dealing with symptoms like acne and irregular cycles for years. Her doctor explained that her high insulin levels caused an increase in androgen production, worsening her PCOS symptoms.
It is not uncommon for women like Lisa to face these challenges, as elevated androgens can interfere with ovulation, making it hard for those with PCOS to conceive (Cleveland Clinic, 2023).
Symptoms of Insulin Resistance in PCOS
PCOS and insulin resistance often go hand in hand and tend to show up with subtle, easy-to-miss signs. These symptoms might feel like everyday annoyances, but they can signal deeper hormonal and metabolic imbalances.
Catching them early helps you manage both PCOS and long-term health risks.
Common Signs to Watch For
Women dealing with PCOS and insulin resistance often report powerful cravings for sweets and starchy foods, especially after meals. Energy crashes—those post-lunch slumps—are also common.
Another telltale sign is stubborn weight gain around the midsection that would not budge, no matter how much you exercise. In some cases, you may also notice dark, velvety patches of skin (acanthosis nigricans) around your neck, groin, or armpits.
These indicators suggest that insulin is not doing its job well, and the body is compensating in unhealthy ways.
Why Testing Matters?
Because these symptoms can mimic other conditions like thyroid issues, chronic stress, or simple fatigue, testing is essential.
The most commonly used methods include a fasting insulin test or a two-hour oral glucose tolerance test (OGTT). You may also make use of a glucometer.
These tests help determine how your body responds to sugar and insulin, catching insulin resistance before it spirals into prediabetes or type 2 diabetes.
Backed by Research
Scientific studies estimate that anywhere from 50% to 80% of women with PCOS have insulin resistance, even if they are not overweight. In fact, lean women with PCOS often go undiagnosed because their weight does not raise alarms.
Certain types of PCOS—especially those with irregular cycles and high androgen levels—are more likely to be linked with insulin resistance.
Beyond the Basics: Other Clues
Additional red flags include increased thirst, frequent urination, fatigue, and recurring yeast infections. These seemingly minor symptoms can be early warnings that your blood sugar and insulin levels are out of balance.
Recognizing these signs empowers you to seek testing and take action—so you can get ahead of the curve, not behind it.
Strategies to Manage Insulin Resistance in PCOS
Managing insulin resistance in PCOS is not just about taking medication; it is a holistic approach involving lifestyle changes, medical interventions, and dietary adjustments:
Exercise Regularly: Engaging in moderate physical activity can enhance the body’s insulin sensitivity. Studies show that exercises like strength training and interval workouts can significantly reduce insulin levels, making it easier to manage weight and PCOS symptoms (Cleveland Clinic, 2023).
Adopt a Low-Glycemic Diet: Reducing carbohydrate intake and focusing on high-fiber foods, lean proteins, and healthy fats can help stabilize blood sugar levels. This approach not only combats insulin resistance but also supports sustainable weight loss—essential for those struggling with “insulin resistance PCOS weight loss.”
Medications: For some, medications like metformin tablets are prescribed to improve insulin sensitivity and lower blood sugar levels. These medications can also help regulate menstrual cycles and reduce androgen levels, alleviating some of the most common PCOS symptoms (Imaware, 2023).
Stress Management: Chronic stress can exacerbate insulin resistance. Techniques such as yoga, meditation, or even walking outdoors can reduce stress hormone levels, thus improving insulin sensitivity.
Breaking the Cycle
PCOS and insulin resistance are locked in a complicated dance where one issue aggravates the other.
Understanding the connection between “pcos and insulin levels” is crucial for effective management.
While there is no cure for PCOS, addressing insulin resistance through a combination of lifestyle changes, diet, opting for behavioral therapy and medical interventions can significantly reduce symptoms and improve quality of life.
The key takeaway is that tackling insulin resistance early is vital.
If you suspect insulin resistance, consult a healthcare professional for testing and treatment options tailored to your needs.
By taking proactive steps, learning how to lower blood sugar naturally, you can manage your PCOS symptoms more effectively and reduce the long-term risks associated with this condition.
References: