How Recessive Mutations in the GCK Gene Lead to Neonatal Diabetes?
- admin
- December 23, 2024
- 8:33 am
- No Comments
Neonatal diabetes is a rare condition that manifests within the first six months of life, characterized by hyperglycemia and insulin deficiency.
Among its genetic causes, recessive mutations in the glucokinase (GCK) gene play a crucial role.
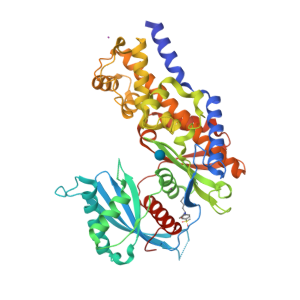
The GCK gene encodes glucokinase, an enzyme that functions as the glucose sensor of pancreatic beta cells.
Its mutations disrupt glucose sensing, impairing insulin secretion and leading to hyperglycemia.
In this article, we will explore how recessive mutations in the GCK gene contribute to neonatal diabetes, examining their molecular mechanisms, clinical presentations, and real-life case studies.
Table of Contents:
- Introduction to the GCK Gene and Its Role in Beta-Cell Function
- Molecular Mechanisms of GCK Mutations
- Glucose Sensing in Beta Cells
- Loss-of-Function Mutations in GCK
- Clinical Manifestations of GCK-Related Neonatal Diabetes
- Hyperglycemia and Insulin Deficiency
- Differentiating Between Permanent and Transient Neonatal Diabetes
- Case Studies: Real-Life Impacts of GCK Mutations
- Case 1: Persistent Neonatal Diabetes Due to GCK Mutations
- Case 2: Transient Neonatal Diabetes in a Sibling Pair
- Scientific Evidence Supporting GCK Mutations and Neonatal Diabetes
- Conclusion
Introduction to the GCK Gene and Its Role in Beta-Cell Function
The GCK gene is responsible for encoding glucokinase, a critical enzyme in the glucose-sensing pathway of pancreatic beta cells.
This enzyme catalyzes the conversion of glucose into glucose-6-phosphate, the initial step in glycolysis.
By regulating this process, glucokinase serves as the primary sensor that links blood glucose levels to insulin secretion, ensuring a balanced response to fluctuations in glucose concentration.
Mutations in the GCK gene disrupt this finely tuned mechanism. Such mutations impair glucokinase’s ability to metabolize glucose, leading to insufficient ATP production.
Without adequate ATP, the insulin secretion cascade is halted, resulting in hyperglycemia.
While heterozygous mutations in GCK are associated with maturity-onset diabetes of the young (MODY) due to mild enzyme dysfunction, more severe homozygous or compound heterozygous mutations cause neonatal diabetes.
In neonates, this manifests as early-onset hyperglycemia, requiring immediate medical intervention, as demonstrated by studies in Nature Genetics (Gloyn et al., 2004).
Molecular Mechanisms of GCK Mutations
A quick look at this:
Glucose Sensing in Beta Cells:
In pancreatic beta cells, glucokinase acts as a glucose sensor, pivotal for regulating insulin secretion.
The enzyme catalyzes the conversion of glucose into glucose-6-phosphate, a critical step in glycolysis.
This process sets the glucose threshold for insulin release, ensuring that insulin secretion corresponds accurately with blood glucose levels to maintain glucose homeostasis.
Loss-of-Function Mutations in GCK:
Recessive mutations in the GCK gene disrupt glucokinase function, typically by reducing its catalytic efficiency or altering its glucose affinity.
These mutations impair the enzyme’s ability to phosphorylate glucose, resulting in reduced ATP production.
Consequently, ATP-sensitive potassium (KATP) channels remain open, preventing the cell membrane from depolarizing.
This lack of depolarization blocks calcium influx, which is essential for triggering insulin granule exocytosis, leading to insulin deficiency and hyperglycemia.
Research by Osbak et al. (2009) in Diabetes provided critical insights into how specific GCK mutations diminish the enzyme’s kinetic efficiency, leading to severe beta-cell dysfunction.
This study emphasized the direct impact of GCK mutations on neonatal diabetes, linking impaired glucose sensing to inadequate insulin secretion.
Clinical Manifestations of GCK-Related Neonatal Diabetes
Here is what you can expect:
Hyperglycemia and Insulin Deficiency:
Neonates with GCK-related neonatal diabetes experience persistent hyperglycemia due to insufficient insulin secretion, as beta cells fail to respond effectively to rising blood glucose levels.
Clinically, affected infants often exhibit symptoms such as excessive thirst (polydipsia), dehydration, and failure to thrive.
Hyperglycemia is frequently the first detectable sign of beta-cell dysfunction, prompting further investigation into the underlying cause.
Differentiating Between Permanent and Transient Neonatal Diabetes:
Mutations in the GCK gene can lead to either transient neonatal diabetes mellitus (TNDM) or permanent neonatal diabetes mellitus (PNDM).
In TNDM, hyperglycemia resolves within the first few months of life but may re-emerge later due to progressive beta-cell dysfunction. In contrast, PNDM is a lifelong condition requiring continuous insulin therapy.
The progression of the disease largely depends on the specific mutation’s severity.
Studies such as those by Edghill et al. (2008) in Human Molecular Genetics emphasize the importance of identifying the mutation type to predict disease outcomes and optimize management strategies.
Persistent Neonatal Diabetes Due to GCK Mutations
Maria, a two-month-old infant, presented with persistent hyperglycemia during a routine pediatric check-up, prompting further investigation.
Genetic testing revealed a homozygous loss-of-function mutation in the GCK gene, severely impairing her glucokinase enzyme activity.
This dysfunction disrupted glucose sensing in her pancreatic beta cells, leading to permanent neonatal diabetes mellitus (PNDM). Maria required insulin therapy to manage her blood glucose levels effectively.
Her case highlights the critical role of early genetic testing in identifying underlying causes of neonatal hyperglycemia, enabling timely interventions to improve metabolic control and prevent complications associated with untreated diabetes in infants.
Transient Neonatal Diabetes in a Sibling Pair:
In a family with two affected siblings, genetic analysis identified compound heterozygous mutations in the GCK gene, confirming the genetic basis for their condition.
Both children were diagnosed with transient neonatal diabetes mellitus (TNDM) shortly after birth, with symptoms resolving by six months of age.
However, during adolescence, both siblings experienced a recurrence of hyperglycemia, underscoring the biphasic nature of TNDM linked to GCK mutations.
This case emphasizes the variability in disease progression and the critical need for long-term monitoring in families with GCK mutations to anticipate and manage potential re-emergence of diabetes later in life.
Scientific Evidence Supporting GCK Mutations and Neonatal Diabetes
- Osbak et al., 2009 (Diabetes): This foundational study detailed how specific loss-of-function GCK mutations impair the enzymatic activity of glucokinase. Researchers demonstrated the link between reduced kinetic efficiency of glucokinase and severe beta-cell dysfunction, establishing these mutations as a direct cause of neonatal diabetes.
- Gloyn et al., 2004 (Nature Genetics): Highlighting recessive mutations in the GCK gene, this study confirmed their role in permanent neonatal diabetes mellitus (PNDM). It emphasized the gene’s critical importance in maintaining glucose homeostasis and beta-cell function.
- Stanley et al., 2016 (Journal of Clinical Endocrinology & Metabolism): This research explored the clinical variability of GCK-related neonatal diabetes, highlighting how different mutations lead to varying disease progression, from transient neonatal diabetes mellitus (TNDM) to lifelong PNDM.
- Rutter et al., 2010 (Endocrine Reviews): This review investigated how defective glucokinase impairs ATP production, disrupting the glucose-sensing mechanism in beta cells. It demonstrated how this impairment prevents adequate insulin secretion, contributing to persistent hyperglycemia.
Conclusion
Recessive mutations in the GCK gene unravel a fascinating glimpse into the genetic intricacies of neonatal diabetes.
These mutations derail the delicate balance of glucose sensing and insulin secretion, causing profound metabolic disturbances.
For families grappling with this condition, early genetic testing becomes a lifeline, enabling timely interventions such as tailored insulin therapy.
The promise of advanced treatments, including gene-editing technologies, adds a layer of optimism.
Scientific research continues to illuminate the molecular dance behind GCK mutations, paving the way for precise diagnostic tools and innovative solutions, offering hope for brighter outcomes for neonates and their families alike.
References: