How Underdeveloped Pancreas Leads to Neonatal Diabetes?
- admin
- December 16, 2024
- 11:02 am
- No Comments
The pancreas plays a critical role in regulating blood glucose levels, primarily through the production of insulin by beta cells.
In neonates, an underdeveloped pancreas can disrupt this process, leading to a rare condition known as neonatal diabetes mellitus (NDM).
Neonatal diabetes, which manifests within the first six months of life, can either be transient (TNDM) or permanent (PNDM).
This article explores how and why an underdeveloped pancreas contributes to neonatal diabetes, examining the biological mechanisms, genetic factors, and real-world examples that highlight the challenges faced by affected individuals and their families.
Article Index:
- The Role of the Pancreas in Glucose Regulation
- Understanding pancreatic development and function
- Importance of insulin in neonatal glucose homeostasis
- How Pancreatic Underdevelopment Causes Neonatal Diabetes
- Impaired beta-cell development
- Insufficient insulin production
- Endocrine versus exocrine pancreatic deficiencies
- Genetic Factors Contributing to Pancreatic Underdevelopment
- Mutations in key regulatory genes
- Syndromic and nonsyndromic forms of neonatal diabetes
- Clinical Implications and Real-Life Case Studies
- Case Study 1: Neonatal diabetes caused by PDX1 mutation
- Case Study 2: Syndromic neonatal diabetes with pancreatic hypoplasia
- Scientific Studies Linking Pancreatic Underdevelopment and Neonatal Diabetes
- Key research findings
- FAQS on Underdeveloped Pancreas and Neonatal Diabetes
- Conclusion
- Summarizing the impact of underdeveloped pancreas on neonatal diabetes
The Role of the Pancreas in Glucose Regulation
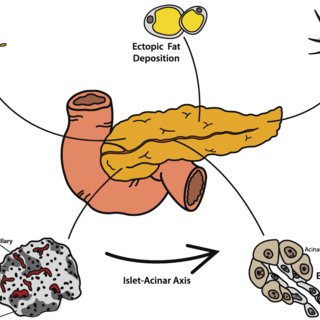
The pancreas is a critical organ with two primary functions:
- Exocrine Function: It produces digestive enzymes necessary for breaking down nutrients in food, facilitating nutrient absorption.
- Endocrine Function: It secretes hormones, predominantly insulin, which regulates blood glucose levels.
In neonates, insulin secretion plays a vital role in managing glucose levels derived from maternal milk.
The beta cells located in the pancreatic islets of Langerhans are responsible for insulin production.
These specialized cells must mature and function optimally during fetal development to ensure effective glucose homeostasis after birth.
An underdeveloped pancreas impairs this essential process.
Without adequate beta-cell mass or functionality, insulin production becomes insufficient, leading to hyperglycemia—a defining characteristic of neonatal diabetes.
This disruption affects the neonate’s ability to process glucose efficiently, emphasizing the critical importance of proper pancreatic development for metabolic health from birth.
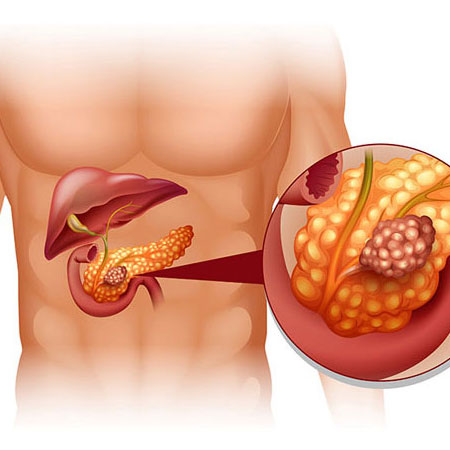
How Pancreatic Underdevelopment Causes Neonatal Diabetes
Here is how it all happens:
Impaired Beta-Cell Development:
Fetal development of the pancreas is a finely tuned process that relies on the coordinated action of transcription factors and signaling pathways.
Regulatory genes like PDX1 and HNF1B play pivotal roles in guiding progenitor cells to differentiate into functional beta cells.
During this phase of organogenesis, any disruption caused by genetic mutations can significantly reduce the beta-cell mass.
An underdeveloped pancreas, lacking sufficient beta cells, is unable to meet the insulin demands of the neonate, creating the foundation for neonatal diabetes.
Insufficient Insulin Production:
The beta cells in the pancreas are responsible for producing insulin, the hormone essential for regulating blood glucose levels.
When beta-cell development is impaired, insulin secretion becomes inadequate. This leads to a state of hyperglycemia, where glucose remains in the bloodstream rather than entering cells for energy production.
Persistent hyperglycemia in neonates, a hallmark of neonatal diabetes, results in poor growth and other metabolic disturbances.
Endocrine Versus Exocrine Pancreatic Deficiencies:
In certain cases of pancreatic underdevelopment, both endocrine (hormone-producing) and exocrine (enzyme-producing) functions are compromised.
The endocrine deficiency affects insulin production, while the exocrine deficiency impairs the secretion of digestive enzymes necessary for nutrient absorption.
This dual impact exacerbates neonatal health issues, as poor nutrient absorption compounds the challenges posed by hyperglycemia, leading to severe weight loss and developmental delays.
Understanding the interplay of these deficiencies is critical in managing neonatal diabetes effectively.
Genetic Factors Contributing to Pancreatic Underdevelopment
Let me walk you through these in brief:
Mutations in Key Regulatory Genes:
Genetic mutations play a pivotal role in pancreatic underdevelopment, particularly those affecting key regulatory genes crucial for pancreatic formation and function:
- PDX1: This gene is vital for early pancreatic development and beta-cell differentiation. Mutations here impair the pancreas’s ability to produce insulin, leading to neonatal diabetes.
- HNF1B: Known for its role in organogenesis, mutations in HNF1B disrupt beta-cell function and contribute to conditions like pancreatic hypoplasia.
- GATA6: This gene is associated with syndromic diabetes and pancreatic hypoplasia, where multiple organ systems may be affected.
These mutations interrupt developmental pathways, resulting in an underdeveloped pancreas and insulin deficiency.
Syndromic and Nonsyndromic Forms:
Genetic mutations may manifest in syndromic or nonsyndromic forms of pancreatic hypoplasia.
Syndromic forms often present alongside other abnormalities, such as kidney malformations or developmental delays. For example, HNF1B mutations commonly result in MODY5 (Maturity-Onset Diabetes of the Young, Type 5), where neonatal diabetes is accompanied by renal cysts and kidney disease.
Conversely, nonsyndromic forms typically involve isolated pancreatic underdevelopment without systemic involvement, emphasizing the diverse presentations of genetic mutations in neonatal diabetes.
Clinical Implications and Real-Life Case Studies
Let’s take a closer look at these:
Case Study: Neonatal Diabetes Caused by PDX1 Mutation:
Emma, a three-month-old infant, presented with persistent hyperglycemia and failure to thrive. Genetic testing revealed a mutation in the PDX1 gene, a crucial regulator of beta-cell development in the pancreas.
This mutation severely impaired the formation and function of insulin-producing beta cells, leading to inadequate insulin secretion. Initially managed with insulin therapy,
Emma’s condition stabilized with the early introduction of sulfonylureas, a class of oral medications that enhanced her remaining beta-cell activity.
Over time, her glucose levels improved, highlighting the effectiveness of timely intervention.
Emma’s case underscores the critical role of PDX1 in pancreatic organogenesis and demonstrates how targeted therapy can improve outcomes for neonates with genetic forms of diabetes.
Syndromic Neonatal Diabetes with Pancreatic Hypoplasia:
Tom, a six-month-old baby, exhibited symptoms of neonatal diabetes alongside renal cysts.
Genetic analysis identified a mutation in the HNF1B gene, linking his condition to syndromic diabetes with pancreatic hypoplasia.
The mutation not only disrupted pancreatic development but also caused renal abnormalities, illustrating the systemic impact of HNF1B mutations.
Tom’s treatment involved a carefully tailored insulin regimen to manage his glucose levels, alongside multidisciplinary care to monitor his kidney health.
This case highlights the importance of comprehensive genetic screening in identifying syndromic conditions and tailoring interventions to address both diabetes and associated complications.
Scientific Studies Linking Pancreatic Underdevelopment and Neonatal Diabetes
Several landmark studies have explored the genetic underpinnings of neonatal diabetes caused by pancreatic underdevelopment:
- Støy et al., 2007 (Diabetologia): This study demonstrated how mutations in the INS gene disrupt proinsulin folding, leading to impaired insulin production. It emphasized the direct link between INS mutations and pancreatic hypoplasia in neonates, providing a foundation for understanding monogenic diabetes.
- Edghill et al., 2008 (Human Molecular Genetics): The research highlighted mutations in the PDX1 gene, a key regulator of beta-cell differentiation. It showed how these mutations impair pancreatic organogenesis and beta-cell development, contributing significantly to neonatal diabetes.
- Molven et al., 2008 (Human Mutation): This study focused on GATA6 mutations, revealing their role in syndromic neonatal diabetes associated with pancreatic and other organ insufficiencies. It shed light on how these mutations disrupt normal organ development.
- Colombo et al., 2010 (Diabetes): Researchers detailed how HNF1B mutations impact pancreatic and renal development, demonstrating their dual role in neonatal diabetes and renal cystic disease. This study highlighted the syndromic nature of some genetic mutations linked to diabetes.
Together, these studies underscore the importance of genetic testing in diagnosing and managing neonatal diabetes caused by pancreatic underdevelopment.
FAQS on Underdeveloped Pancreas and Neonatal Diabetes
Q-1: What does an “underdeveloped pancreas” mean, and why can it cause diabetes in the first 6 months?
A-1: It means the pancreas forms too small (hypoplasia) or is nearly absent (agenesis). With too few or immature insulin-producing β-cells at birth, the infant cannot release enough insulin to control blood sugar, so persistent hyperglycemia appears in early infancy. Because the exocrine portion may also be undersized, some babies show fat malabsorption, poor weight gain, or greasy stools alongside high glucose.
Q-2: Which early clues suggest a developmental problem rather than autoimmune diabetes?
A-2: Hallmarks include diagnosis before 6 months, low birth weight or intrauterine growth restriction, negative islet autoantibodies, and signs of malabsorption. C-peptide may still be detectable but is inappropriately low for the glucose level. Imaging (ultrasound or MRI) that shows a very small or absent pancreas strengthens the case for a developmental cause instead of typical autoimmune disease.
Q-3: Which genes are commonly involved when the pancreas is underdeveloped?
A-3: Changes in key transcription-factor genes that guide organ formation are often implicated. Variants in GATA6, PDX1, or PTF1A frequently present with neonatal diabetes, and some also produce exocrine insufficiency or extra-pancreatic features (such as cardiac or biliary anomalies). Broader testing may include RFX6, HNF1B, and select metabolic or channel genes to capture the full spectrum.
Q-4: How do clinicians confirm the diagnosis and distinguish it from other neonatal diabetes forms?
A-4: The evaluation is stepwise: document persistent hyperglycemia in early infancy, check islet autoantibodies, assess exocrine function with fecal elastase, and image the pancreas. Genetic testing then pinpoints the mechanism. Finding, for example, a GATA6 or PTF1A variant together with pancreatic hypoplasia/agenesis supports a developmental origin rather than a defect in insulin secretion pathways like KATP-channel disorders.
Q-5: What does management look like when pancreatic underdevelopment is the root cause?
A-5: Care must address both endocrine and exocrine roles. Insulin therapy manages hyperglycemia. If malabsorption is present, pancreatic enzyme replacement and fat-soluble vitamins support growth. Practical steps include caregiver education on insulin dosing and hypoglycemia prevention, optimized formula or breastfeeding plans, and close follow-up with endocrinology, gastroenterology, and nutrition teams to track growth and developmental milestones.
Q-6: Why are low birth weight and feeding issues common, and what is the long-term outlook?
A-6: Fetal insulin is an important growth factor; with fewer β-cells in utero, babies often arrive small for gestational age. After birth, exocrine insufficiency can further hinder weight gain without enzyme therapy. Long-term outcomes vary by the gene involved and any associated organ findings, but with timely diagnosis, appropriate insulin management, and enzyme support when needed, many children achieve catch-up growth and stable metabolic control.
Conclusion
An underdeveloped pancreas is a critical factor in the onset of neonatal diabetes, as it directly impairs beta-cell development and leads to inadequate insulin production.
This underdevelopment is often rooted in genetic mutations in key regulatory genes such as PDX1, HNF1B, and GATA6, which play pivotal roles in pancreatic organogenesis.
Mutations in these genes disrupt the normal formation and function of beta cells, leaving neonates unable to regulate blood glucose levels effectively.
For example, mutations in PDX1 affect the differentiation of beta cells, while HNF1B mutations can impair not only the pancreas but also renal development, leading to syndromic complications.
Similarly, GATA6 mutations are associated with pancreatic insufficiency and other systemic abnormalities.
As per bestdietarysupplementfordiabetics.com, “Early diagnosis through advanced genetic testing is crucial for identifying the specific mutations responsible and tailoring interventions to manage the condition effectively”.
By addressing these genetic and developmental challenges, clinicians can improve long-term outcomes for neonates and expand our understanding of the intricate mechanisms that govern pancreatic development and its link to diabetes.
References: