Is Hyperglycemia the Real Culprit Behind Steroid Induced Diabetes?
- admin
- September 26, 2024
- 4:07 pm
- No Comments
Steroids can be a double-edged sword. They are lifesavers for managing conditions like inflammation, asthma, and autoimmune diseases but can also bring some unwelcome side effects.
Among these, steroid-induced diabetes mellitus stands out as a serious concern.
But what is really going on here?
Is hyperglycemia—the fancy term for high blood sugar—truly to blame for this condition?
Or is there more beneath the surface?
In this article, I shall explore the complex relationship between steroids and diabetes, looking closely at how steroids affect blood sugar and what you can do to manage this condition effectively.
Article Index:
- Understanding Steroid-Induced Diabetes Mellitus
- The Role of Hyperglycemia in Steroid-Induced Diabetes
- Steroid-Induced Hyperglycemia Mechanism: How Does It Happen?
- Diagnostic Criteria for Steroid-Induced Diabetes
- Steroid-Induced Hyperglycemia Management and Treatment
- Best Diet for Steroid-Induced Diabetes
- Lifestyle Adjustments and Reversing Steroid-Induced Diabetes
- Combining Medications and Lifestyle: A Comprehensive Approach
- FAQs on Hyperglycemia & Diabetes
- Conclusion: Is Hyperglycemia the True Culprit?
Understanding Steroid-Induced Diabetes Mellitus
Steroid-induced diabetes mellitus is a type of diabetes that occurs in people taking corticosteroids like prednisone.
These medications are often prescribed for conditions such as asthma, rheumatoid arthritis, and lupus.
While they are incredibly effective at reducing inflammation, they can also cause blood sugar levels to skyrocket, leading to what we call steroid-induced hyperglycemia.
If left unmanaged, this can progress to full-blown diabetes.
But why do steroids have this effect?
It all comes down to how they interact with your body’s glucose metabolism.
Corticosteroids work by mimicking the hormone cortisol, which your adrenal glands naturally produce.
Cortisol is involved in several body processes, including your stress response, immune system regulation, and crucially, glucose metabolism.
High doses or long-term use of steroids can disrupt this delicate balance, leading to elevated blood sugar levels and, eventually, diabetes.
The Role of Hyperglycemia in Steroid-Induced Diabetes
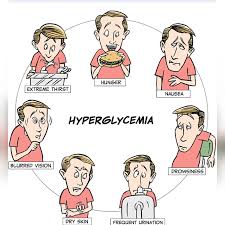
So, what exactly is hyperglycemia?
Hyperglycemia occurs when your blood sugar levels are higher than normal.
When this condition is triggered by steroids, it’s called steroid-induced hyperglycemia.
If this state persists, it can evolve into steroid-induced diabetes mellitus.
But is hyperglycemia the true culprit here, or is it just a symptom of a more complex issue?
The connection between steroids and hyperglycemia is straightforward but problematic.
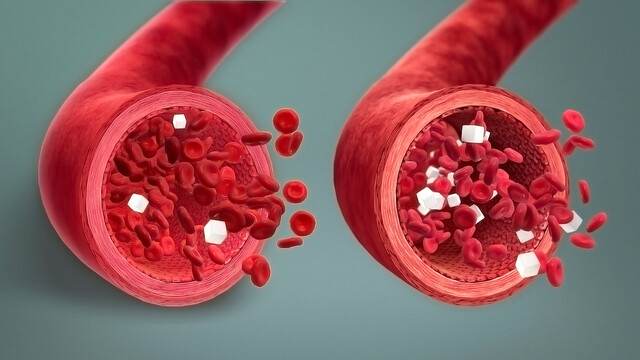
Steroids can increase glucose production in your liver while making it harder for your body to use insulin effectively, a condition known as insulin resistance.
This dual action leads to high blood sugar levels, particularly after meals—a phenomenon known as postprandial hyperglycemia.
But to truly understand whether hyperglycemia is the main villain in the story of steroid-induced diabetes, we need to dive deeper into the mechanisms at play.
Steroid-Induced Hyperglycemia Mechanism: How Does It Happen?
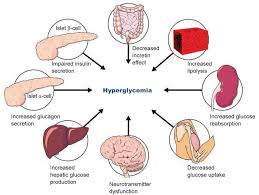
The mechanism of steroid-induced hyperglycemia involves several complex pathways:
1. Increased Gluconeogenesis:
Steroids stimulate the liver to produce more glucose, a process known as gluconeogenesis.
This is essentially your body creating new glucose from non-carbohydrate sources like amino acids.
While this is beneficial in short bursts (think fight-or-flight scenarios), long-term steroid use can lead to consistently high glucose production, overwhelming your body’s ability to regulate blood sugar.
2. Reduced Insulin Sensitivity:
Steroids make your body’s cells less responsive to insulin, a condition known as insulin resistance.
This means your body needs to produce more insulin to keep blood sugar levels in check.
Over time, your pancreas may struggle to keep up with this demand, leading to elevated blood sugar levels.
3. Decreased Insulin Secretion:
In some cases, steroids can directly impair the pancreas’s ability to secrete insulin.
This further exacerbates the problem of high blood sugar, as your body lacks the insulin needed to regulate glucose levels effectively.
4. Altered Fat and Protein Metabolism:
Steroids also influence how your body metabolizes fats and proteins, leading to increased free fatty acids and amino acids in the bloodstream.
This metabolic disruption can contribute to weight gain and further insulin resistance, making it even harder to control blood sugar levels.
Understanding these mechanisms is crucial for effective management of steroid-induced hyperglycemia.
Diagnostic Criteria for Steroid-Induced Diabetes
How do you know if your high blood sugar has crossed the line into steroid-induced diabetes?
The steroid-induced diabetes diagnostic criteria are similar to those for other types of diabetes but come with their nuances due to the unique impact of steroids on blood sugar.
Fasting Blood Glucose Levels: A fasting blood sugar level of 126 mg/dL or higher on two separate occasions is a clear indicator of diabetes.
Random Blood Glucose Levels: A random blood sugar level of 200 mg/dL or higher, accompanied by symptoms like increased thirst and urination, can indicate diabetes.
HbA1c Levels: An HbA1c level of 6.5% or higher suggests diabetes. However, steroids can cause fluctuations in HbA1c levels, making this test less reliable in people taking steroids.
Oral Glucose Tolerance Test (OGTT): This test measures your blood sugar levels before and after consuming a glucose-rich drink. A result of 200 mg/dL or higher two hours after drinking the solution indicates diabetes.
These criteria help doctors determine whether you have transitioned from steroid-induced hyperglycemia to steroid-induced diabetes mellitus.
Steroid-Induced Hyperglycemia Management and Treatment
Managing steroid-induced hyperglycemia is not as simple as cutting out carbs or exercising more, although both of those things help.
It requires a multifaceted approach that includes medication, monitoring, and lifestyle changes.
Medication:
Insulin: For some people, especially those with high blood sugar levels, insulin may be necessary to bring glucose levels under control.
Metformin: Often the first line of defense, metformin helps improve insulin sensitivity and reduce glucose production in the liver.
DPP-4 Inhibitors and SGLT2 Inhibitors: These medications can also be useful in managing glucocorticoid-induced hyperglycemia by improving insulin sensitivity and promoting glucose excretion through urine.
Monitoring:
Regular monitoring is crucial for effective steroid-induced hyperglycemia treatment.
This includes frequent blood sugar checks, especially after meals, and periodic HbA1c tests to gauge long-term control.
If you are taking steroids and your blood sugar levels are high, your doctor may recommend continuous glucose monitoring (CGM) to provide a more detailed picture.
Best Diet for Steroid-Induced Diabetes
Your diet plays a significant role in managing steroid-induced hyperglycemia. But what exactly is the best diet for steroid-induced diabetes?
Focus on Low-Glycemic Index Foods:
Low-glycemic index foods like whole grains, legumes, and most vegetables have a slower, more gradual impact on blood sugar levels.
They are less likely to cause the spikes and crashes associated with high-glycemic foods like white bread and sugary snacks.
Include Lean Proteins and Healthy Fats:
Lean proteins like chicken, turkey, and fish, along with healthy fats from sources like avocados, nuts, and olive oil, can help stabilize blood sugar levels.
They also make meals more satisfying, reducing the temptation to overeat.
Avoid Simple Sugars and Refined Carbohydrates:
Simple sugars and refined carbohydrates can cause your blood sugar levels to spike rapidly, which is especially problematic for those dealing with steroid-induced hyperglycemia.
Steer clear of sugary snacks, sodas, and processed foods.
Portion Control and Meal Timing:
Eating smaller, more frequent meals can help maintain more stable blood sugar levels throughout the day.
Pairing carbohydrates with protein or fat can also slow down glucose absorption, preventing rapid spikes.
Lifestyle Adjustments and Reversing Steroid-Induced Diabetes
A quick look at how minor adjustments to your daily routine can make a dramatic impact on your blood sugar levels:
Physical activity can improve insulin sensitivity and help lower blood sugar levels.
Aim for at least 30 minutes of moderate exercise most days of the week.
Activities like brisk walking, cycling, and swimming are excellent choices.
Stress Management:
Chronic stress can elevate cortisol levels, compounding the effects of steroids on your blood sugar.
Techniques like meditation, deep breathing, and yoga can help manage stress and keep your blood sugar levels in check.
Sleep Hygiene:
Lack of sleep can worsen insulin resistance and increase your risk of developing diabetes.
Aim for 7-9 hours of quality sleep per night.
Combining Medications and Lifestyle: A Comprehensive Approach
Effectively managing steroid-induced hyperglycemia often requires a combination of medication and lifestyle changes.
For instance, you might take insulin or metformin to manage your blood sugar levels while also following a diet and diabetes control exercise plan tailored to your needs.
Regular follow-ups with your healthcare provider are crucial for monitoring your progress and adjusting your treatment plan as needed.
This comprehensive approach can help you achieve better control over your blood sugar levels and minimize the long-term impact of steroids on your health.
FAQs on Hyperglycemia & Diabetes
Q-1: Is hyperglycemia the main reason steroid-induced diabetes develops?
A-1: Hyperglycemia is the most visible sign of steroid-induced diabetes, but it’s more of a result than a single cause. Steroids push the liver to release extra glucose, reduce how effectively muscles use sugar, and interfere with insulin’s normal action.
These changes raise blood sugar levels repeatedly. When this high blood sugar persists, it creates a diabetes-like state. So, hyperglycemia is the final trigger, but it is driven by deeper metabolic changes caused by steroid use.
Q-2: Why do some people develop diabetes from steroids while others don’t?
A-2: Individual risk plays a big role. People who already have insulin resistance, prediabetes, a family history of diabetes, or higher body fat are more vulnerable to steroid effects.
For others, the pancreas can compensate by releasing more insulin, keeping blood sugar under control. When that compensation fails, hyperglycemia becomes persistent and diabetes develops.
Q-3: Can steroid-related hyperglycemia damage the pancreas itself?
A-3: Yes. When blood sugar stays high for long periods, beta cells in the pancreas are forced to work overtime to produce insulin. This constant strain can exhaust them and reduce their ability to function effectively. Over time, this may cause insulin production to drop, making high blood sugar harder to reverse even after steroid treatment ends.
Q-4: Is steroid-induced hyperglycemia always temporary?
A-4: In many cases, it is temporary — especially when steroids are used for short periods. Once the medication is reduced or stopped, blood sugar often returns to normal. As per bestdietarysupplementfordiabetics.com.
However, in people with underlying metabolic risk, steroids can uncover or accelerate the development of long-term type 2 diabetes. In these cases, blood sugar may remain elevated even after steroid therapy ends.
Q-5: Does the timing of blood sugar spikes matter in steroid-induced diabetes?
A-5: Yes, timing matters a lot. Steroids often cause blood sugar to rise after meals and later in the day rather than during fasting. These repeated post-meal spikes increase average blood sugar levels and stress insulin-producing cells.
If only fasting glucose is checked, steroid-induced diabetes may be missed, allowing hyperglycemia to continue unnoticed.
Takeaway: Is Hyperglycemia the True Culprit?
So, is hyperglycemia the real culprit behind steroid-induced diabetes mellitus?
While hyperglycemia plays a significant role, it is not the root cause.
The true issue is how steroids disrupt your body’s normal glucose metabolism, leading to elevated blood sugar levels as a consequence.
Hyperglycemia is more of a symptom than a cause in this complex interplay.
Understanding the steroid-induced hyperglycemia mechanism is key to effective management.
Whether you are dealing with temporary steroid treatment or long-term use, knowing how to monitor and control your blood sugar can make a world of difference.
Ultimately, managing steroid-induced diabetes involves a balance of blood sugar support supplement, diet, exercise, and continuous blood sugar monitoring.
By adopting a holistic approach, you can minimize the impact of steroids on your blood sugar levels and maintain better overall health.
References: