Is Insulin Infusion Pump the Hidden Danger in Diabetes Treatment?
- admin
- September 28, 2024
- 7:41 pm
- No Comments

Insulin pumps have revolutionized diabetes management, offering a convenient and effective way to regulate blood sugar levels without the need for multiple daily injections.
But as with any medical device, insulin pumps are not without their drawbacks.
From the risk of infections to potential technology malfunctions, some experts are beginning to question whether insulin infusion pumps are truly the panacea they’re made out to be.
Could these devices, designed to ease the burden of diabetes, actually be a hidden danger in treatment?
Let’s delve into the pros and cons of insulin pump therapy to find out.
This Article Includes:
- What is Insulin Pump Therapy?
- How Insulin Pumps Work: The Basics
- The Pros and Cons of Insulin Pump Treatment
- The Hidden Risks of Continuous Subcutaneous Infusion Pumps
- Infection Risks: A Cause for Concern?
- Managing Insulin Pump Infections
- Are There Safer Alternatives?
- Conclusion: Is the Insulin Pump a Friend or Foe?
What is Insulin Pump Therapy?
Insulin pump therapy is a modern approach to diabetes management that uses a small, computerized device to deliver insulin in a steady, controlled manner.
This method is known as Continuous Subcutaneous Insulin Infusion (CSII) and is designed to closely replicate how a healthy pancreas naturally releases insulin throughout the day and in response to meals.
Unlike traditional insulin injections—which often involve multiple daily shots with varying doses—an insulin pump provides a basal dose (background insulin) around the clock and bolus doses at mealtimes.
The pump connects to the body through a thin, flexible tube called a catheter, which is inserted just under the skin, typically in the abdomen, hip, or thigh.
This therapy is especially favored by individuals with type 1 diabetes, as it allows for finer adjustments and can lead to improved glycemic control.
For instance, a student with an unpredictable school schedule or an athlete with fluctuating energy needs can fine-tune insulin delivery to match activity and stress levels—something difficult to do with fixed-dose injections.
Insulin pumps also reduce the frequency of severe highs and lows. Studies show that users often experience lower HbA1c levels, fewer episodes of hypoglycemia, and better quality of life.
Some advanced pumps even integrate with Continuous Glucose Monitors (CGMs) to automate insulin delivery based on real-time blood sugar readings, forming the foundation of what’s now called a hybrid closed-loop system or “artificial pancreas.”
In short, insulin pump therapy offers flexibility, precision, and control—making life with diabetes just a little more predictable..
How Insulin Pumps Work: The Basics
Insulin pumps have transformed diabetes management by offering a more precise, continuous way to deliver insulin without relying on multiple daily injections.
Ideal for individuals with type 1 diabetes—and increasingly for some with type 2—these devices bring flexibility, control, and technological sophistication to blood sugar management.
Here is how insulin pumps work, broken down clearly:
Main components
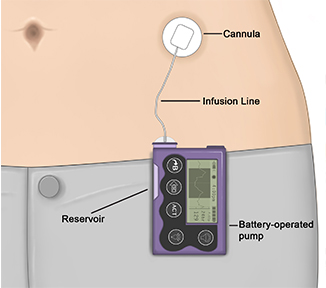
An insulin pump setup includes three parts: the pump (which holds the insulin), a thin tube (called a catheter), and an infusion set that connects to the body. Some newer pumps are tubeless, adhering directly to the skin like a patch.Basal and bolus insulin
The pump delivers a continuous, slow background dose of insulin (basal rate) to mimic the body’s natural release. It can also be programmed to deliver larger bursts (bolus doses) during meals or to correct high blood sugar.Precise programming
Insulin doses can be finely tuned based on time of day, activity level, illness, or sleep patterns. This programmable flexibility often leads to tighter glucose control.Integration with CGMs
Many pumps now work in tandem with continuous glucose monitors (CGMs). This combo can automatically adjust insulin delivery based on real-time glucose data.Improved outcomes
Users often experience better A1C results, fewer hypoglycemic episodes, and a higher quality of life.Tech-savvy designs
Pumps like the Omnipod are tubeless, while others feature smartphone or touchscreen controls. Some newer models even use algorithms that adapt insulin delivery automatically.Cost and care
While insulin pumps require an upfront investment and careful maintenance, their long-term benefits often outweigh these hurdles. They require regular site changes and diligent monitoring to avoid issues like infection or tubing blockage.
With advancing technology and AI-driven systems on the rise, insulin pumps are paving the way toward more intuitive, automated diabetes care.
The Pros and Cons of Insulin Pump Treatment
Pros:
- Improved Blood Sugar Control: Insulin pumps can offer more stable blood glucose levels by delivering insulin more accurately than insulin injections.
- Flexibility and Convenience: The ability to adjust insulin doses on the go provides more freedom in terms of diet and lifestyle.
- Reduced Need for Injections: Patients typically replace the infusion set only every few days, significantly reducing the frequency of needle sticks.
Cons:
- Risk of Infection: As with any device that penetrates the skin, there is a risk of infection at the infusion site.
- Device Malfunction: Mechanical issues or software errors can lead to improper insulin delivery, causing hypo- or hyperglycemia.
- Complexity: Managing an insulin pump requires education and regular monitoring, which can be challenging for some patients.
The Hidden Risks of Continuous Subcutaneous Infusion Pumps
While insulin pumps provide many benefits, they also come with certain risks that can make them a “hidden danger” for some users.
Some diabetics consider insulin pumps as overhyped as they pose far more risks than advantages.
One of the main concerns is the risk of diabetic ketoacidosis (DKA), a serious condition that occurs when the body cannot produce enough insulin.
This risk is heightened if the infusion set becomes dislodged or blocked, stopping insulin delivery.
Another issue is the risk of automatic insulin injection errors, where the pump delivers too much or too little insulin due to technical malfunction.
This can lead to severe fluctuations in blood glucose levels, posing a serious risk to the patient.
Infection Risks: A Cause for Concern?
Infection at the infusion site is one of the most common complications associated with insulin pumps.
Because the catheter remains under the skin for several days, bacteria can enter and cause an infection.
According to a study published in the Journal of Diabetes Science and Technology, the risk of infection increases with the duration of use and poor hygiene practices.
Insulin pump infection treatment typically involves removing the infusion set and applying topical or oral antibiotics.
However, more severe cases may require hospitalization and intravenous antibiotics, especially if the infection spreads.
Managing Insulin Pump Infections
To minimize the risk of infection, it is crucial to follow best practices for insulin pump use. Here are some tips:
- Rotate Infusion Sites: Regularly change the location of the infusion set to prevent skin irritation and scar tissue buildup.
- Use Sterile Techniques: Always wash your hands and clean the skin with an antiseptic before inserting the infusion set.
- Monitor for Signs of Infection: Redness, swelling, or discharge at the infusion site should be reported to your healthcare provider immediately.
In severe cases, insulin pump infection antibiotics may be necessary. These are typically broad-spectrum antibiotics that target the most common bacterial strains responsible for infections.
Are There Safer Alternatives?
For those who find insulin pumps cumbersome or risky, several alternatives exist.
Multiple daily injections (MDI) with a pen or syringe remain a popular option.
Another alternative is the use of automatic glucose monitoring and insulin injection systems, which combine continuous glucose monitoring (CGM) with automatic insulin delivery, reducing the need for user intervention.
Additionally, exploring alternative insulin pump infusion sites can sometimes alleviate discomfort and reduce infection risk.
Sites like the upper thigh or the back of the arm, while less conventional, can provide effective insulin absorption and be easier to manage.
Conclusion: Is the Insulin Pump a Friend or Foe?
So, is the insulin infusion pump the hidden danger in diabetes treatment?
While it certainly has its risks—ranging from infection to device malfunction—these are largely manageable with proper use, regular monitoring and including best dietary supplement for diabetics.
For many, the benefits of improved blood sugar control and lifestyle flexibility far outweigh the potential drawbacks.
However, it is essential for users to be well-informed and vigilant to avoid complications.
Ultimately, whether the insulin pump is a friend or foe depends on individual circumstances and how well the device is managed.
It is not a one-size-fits-all solution, and those considering or currently using an insulin pump should work closely with their healthcare team to ensure it is the right fit for them.
Tip of the Day: By staying informed and proactive, you can make the best decision for your diabetes management and minimize the hidden dangers associated with insulin pump therapy.
References: