Is Pancreatitis the Hidden Cause of Type 3c Diabetes?
- admin
- September 15, 2024
- 6:19 pm
- No Comments
Most of us are familiar with the common types of diabetes, especially type 1 and type 2.
However, type 3c diabetes mellitus (also known as pancreatogenic diabetes) is often overlooked and underdiagnosed.
This type of diabetes arises from damage to the pancreas, frequently linked to pancreatitis or other pancreatic diseases.
But how exactly does pancreatitis lead to type 3c diabetes, and why is it frequently misdiagnosed as type 2 diabetes?
In this article, I will explore the relationship between pancreatitis and type 3c diabetes, diving into the science behind it, the symptoms, and what makes type 3c diabetes so unique.
Contents of “Is Pancreatitis the Hidden Cause of Type 3c Diabetes” Article:
- What is Pancreatitis?
- How Does Pancreatitis Lead to Type 3c Diabetes?
- Signs of Pancreatitis and Its Connection to 3c Diabetes
- Understanding Pancreatogenic Diabetes (Type 3c)
- 7 Symptoms of Pancreas Problems
- Grey Turner Sign and Its Relevance to Pancreatitis
- Diagnosis and Treatment of Type 3c Diabetes
- Conclusion: Is Pancreatitis the Hidden Cause of Type 3c Diabetes?
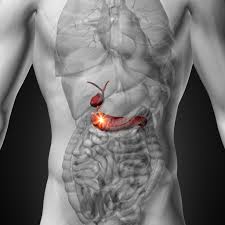
What is Pancreatitis?
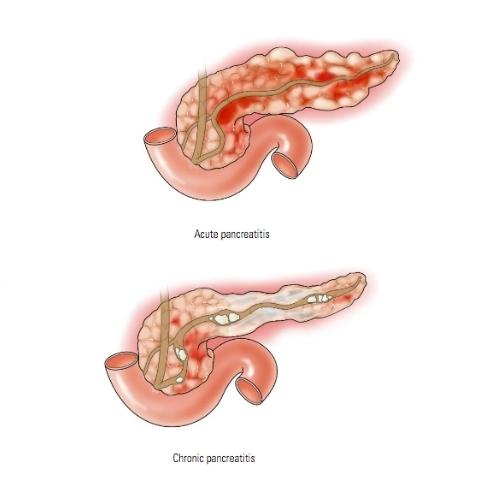
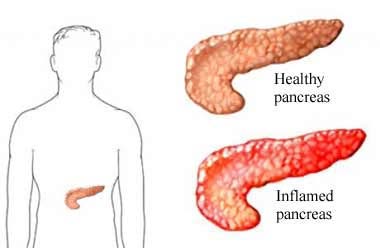
Pancreatitis refers to the inflammation of the pancreas, an organ responsible for producing enzymes that help digest food and hormones that regulate blood sugar, such as insulin.
Pancreatitis can be acute, occurring suddenly and often triggered by gallstones or excessive alcohol consumption, or chronic, where inflammation persists over time, often leading to permanent damage to the pancreas.
When the pancreas becomes inflamed, it fails to perform its normal functions.
Over time, repeated inflammation, particularly in chronic cases, can lead to scarring, tissue damage, and impaired hormone production, which are critical in controlling blood sugar levels.
How Does Pancreatitis Lead to Type 3c Diabetes?
Type 3c diabetes, also known as pancreatogenic diabetes (t3cdm), occurs when pancreatic damage disrupts the organ’s ability to produce insulin.
Unlike type 1 diabetes, where the immune system destroys insulin-producing cells, or type 2 diabetes, where the body becomes resistant to insulin, type 3c diabetes is a result of physical damage to the pancreas.
This damage can be caused by chronic pancreatitis, pancreatic surgery, pancreatic cancer, or cystic fibrosis.
Research published in The Lancet shows that approximately 9% of all diabetes cases are actually type 3c, but this figure is often underestimated because it is frequently misdiagnosed as type 2 diabetes.
A key difference is that individuals with type 3c diabetes often struggle with both the endocrine function (insulin production) and exocrine function (digestive enzyme production) of the pancreas.
This dual dysfunction makes type 3c diabetes distinct and more challenging to manage compared to other forms of diabetes.
Signs of Pancreatitis and Its Connection to 3c Diabetes
Recognizing the signs of pancreatitis early on is crucial for preventing long-term damage that could lead to type 3c diabetes.
The signs of pancreatitis vary depending on whether it’s acute or chronic but often include:
- Upper abdominal pain that radiates to the back
- Nausea and vomiting
- Fever
- Rapid pulse
- Weight loss
- Fatty, foul-smelling stools (due to a lack of digestive enzymes)
When pancreatitis becomes chronic, the repeated damage to the pancreatic cells can trigger the onset of type 3c diabetes.
One hallmark feature of type 3c diabetes is that it appears several years after chronic pancreatitis has been present.
Understanding Pancreatogenic Diabetes (Type 3c)
Pancreatogenic diabetes, or type 3c diabetes mellitus, results from the destruction of both the endocrine and exocrine functions of the pancreas.
As mentioned, this condition is often underdiagnosed, with many patients being incorrectly labeled as having type 2 diabetes.
Yet, the distinction is vital because treatment strategies for type 3c diabetes differ from those for type 2.
According to a 2020 study in Diabetes Care, patients with type 3c pancreatogenic diabetes have more complex needs, as they require both insulin replacement and enzyme supplementation to manage digestive issues.
This is why it is essential for clinicians to distinguish between type 3c diabetes and other forms of diabetes early in the diagnosis process.
7 Symptoms of Pancreas Problems
The pancreas plays a critical role in both digestion and blood sugar regulation.
When it is not functioning properly, the effects can ripple throughout the body—sometimes subtly, other times dramatically.
The following seven symptoms could indicate pancreatic distress, including risks of pancreatitis or type 3c diabetes:
Upper Abdominal Pain after Meals:
Pain that intensifies after eating—particularly in the upper abdomen—is one of the earliest signs of pancreatic inflammation. This pain can also worsen when lying down and may persist for hours.
Back Pain Radiating from the Abdomen:
Pancreatic pain often radiates to the back, especially in chronic conditions. If the pain feels deep, gnawing, and improves slightly when leaning forward, it is worth medical attention.
Unintended Weight Loss:
When the pancreas fails to produce enough digestive enzymes, nutrients aren’t absorbed efficiently. This leads to weight loss despite a regular or even increased appetite.
Steatorrhea (greasy stools):
Fat malabsorption causes stools to appear pale, bulky, and oily. These stools often float and are hard to flush—an indicator of exocrine pancreatic insufficiency.
- Jaundice
Yellowing of the skin or eyes may indicate a bile duct obstruction, often due to inflammation, scarring, or even a tumor pressing on the bile pathway. - Chronic diarrhea
Without adequate enzymes, food isn’t digested properly, leading to frequent, loose stools. Diarrhea often worsens after high-fat meals. - Persistent nausea and vomiting
These symptoms, particularly when coupled with other digestive issues, may point to chronic pancreatic inflammation or functional decline.
If these signs are frequent or long-lasting, they could signal damage to both the digestive and insulin-producing parts of the pancreas—eventually leading to type 3c diabetes.
Early diagnosis and intervention are essential for managing symptoms and preventing complications.
Grey Turner Sign and Its Relevance to Pancreatitis
One lesser-known but important symptom of severe pancreatitis is Grey Turner sign, which refers to bruising on the flanks (the sides of the body between the ribs and hips).
This sign often indicates internal bleeding associated with acute pancreatitis, signaling a serious condition that requires immediate medical attention.
While Grey Turner sign is more commonly seen in acute, severe pancreatitis, its presence indicates the potential for significant pancreatic damage, which could contribute to the development of diabetes mellitus 3c over time.
Diagnosis and Treatment of Type 3c Diabetes
Diagnosing type 3c pancreatogenic diabetes can be tricky because it shares so many characteristics with type 2 diabetes.
However, specific tests, such as imaging studies (CT or MRI scans) to assess pancreatic damage and blood tests to check for exocrine insufficiency (such as low fecal elastase levels), can help differentiate type 3c diabetes from other forms.
Treatment for type 3c diabetes typically involves:
- Insulin therapy: Since the pancreas cannot produce adequate insulin, patients will require insulin replacement to control their blood sugar.
- Digestive enzyme supplements: Given that type 3c diabetes involves exocrine dysfunction, enzyme supplements are often necessary to aid in the digestion of fats and proteins.
- Nutritional support: Patients may also need special diets to compensate for malabsorption, as well as regular monitoring of blood sugar levels.
While these treatment strategies help manage the symptoms, they do not reverse pancreatic damage, emphasizing the importance of early intervention for pancreatitis to prevent the onset of 3c diabetes.
Is Pancreatitis the Hidden Cause of Type 3c Diabetes?
In conclusion, pancreatitis is indeed a significant and often hidden cause of type 3c diabetes mellitus.
Chronic pancreatitis damages the pancreas over time, impairing both insulin and digestive enzyme production, leading to the onset of type 3c diabetes.
Unfortunately, this type of diabetes is often misdiagnosed as type 2, meaning many patients do not receive the proper treatment they need.
Recognizing the early signs of pancreatitis and seeking appropriate medical care can help prevent the progression of pancreatic damage and reduce the risk of developing type iiic diabetes.
If you have experienced chronic pancreatitis or other pancreatic issues, it is essential to speak to your healthcare provider about the possibility of pancreatogenic diabetes.
While there is no cure for type 3c diabetes, early detection, taking a natural Blood Sugar Support Supplement and treatment can improve quality of life and help manage symptoms effectively.
References: