What is the Role of Insulin Hormone in Type 1 Diabetes?
- admin
- October 4, 2024
- 5:28 pm
- No Comments
Type 1 diabetes (T1D) is a complex condition that many people struggle to understand fully.
At the heart of the issue lies a hormone called insulin, which plays a crucial role in regulating blood sugar levels.
But what happens when the body stops producing insulin? And why does this lead to type 1 diabetes?
In this article, I shall dig deep into the role of insulin in type 1 diabetes, explore the science behind it, and provide relatable examples from daily life.
Contents of this Article:
- Introduction to Insulin and Type 1 Diabetes
- What is Insulin?
- How Insulin Works in the Body
- What Happens in Type 1 Diabetes?
- Why Does the Pancreas Stop Producing Insulin?
- Daily Life with Type 1 Diabetes
- Scientific Studies on Insulin and T1D
- Conclusion: The Role of Insulin in Type 1 Diabetes
Introduction to Insulin and Type 1 Diabetes
You have probably heard about insulin in relation to diabetes, but its role is much more than just being “that hormone that diabetics need.”
For people with insulin type 1 diabetes, the hormone’s absence can turn a well-functioning body system into one that requires constant attention, management, and, yes, injections.
Type 1 diabetes occurs when the pancreas is not producing insulin, leaving the body unable to regulate blood sugar.
This might seem like a straightforward cause-effect relationship, but there’s a lot more going on.
Let me now reveal to you what insulin is, why it is so important, and how its absence wreaks havoc in type 1 diabetes.
What is Insulin?
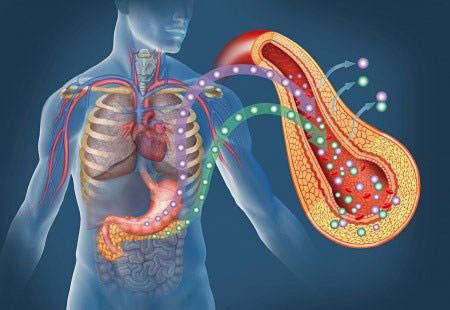
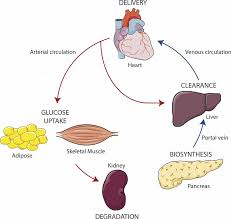
Insulin is a vital hormone that plays a central role in regulating blood sugar levels and overall metabolism. It is produced by specialized cells known as beta cells, which are located within clusters called the islets of Langerhans inside the pancreas.
This small gland, nestled behind the stomach, has both endocrine and exocrine functions, but its role in insulin production is perhaps its most critical contribution to glucose control.
The moment we consume carbohydrates, they are broken down into glucose (sugar), which enters the bloodstream. This spike in blood sugar acts as a signal for the beta cells to release insulin.
Think of insulin as a molecular key—it “unlocks” the doors of muscle, fat, and liver cells, allowing them to absorb glucose from the bloodstream. Once inside the cells, glucose can be used for immediate energy or stored for future use in the form of glycogen.
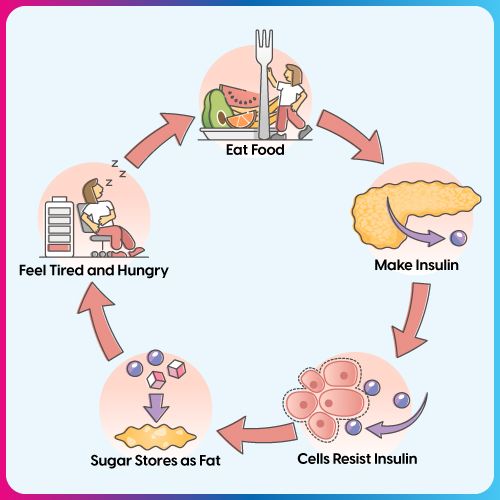
When insulin is absent or insufficient, or when the body’s cells become resistant to its effects, glucose cannot enter the cells efficiently.
Instead, it builds up in the bloodstream—a condition known as hyperglycemia. This is the underlying mechanism in both Type 1 and Type 2 diabetes.
In Type 1 diabetes, the body’s immune system mistakenly attacks and destroys its own beta cells, leading to a complete lack of insulin production. In contrast, Type 2 diabetes typically involves insulin resistance, where the body still produces insulin, but the cells don’t respond to it properly.
Over time, chronically high blood sugar can damage organs and systems throughout the body, including the eyes, kidneys, nerves, and heart. Understanding how insulin functions is crucial not only for managing diabetes but also for preventing its long-term complications.
It is a tiny hormone with a massive impact on health and energy regulation.
How Insulin Works in the Body?
Under normal circumstances, insulin regulates the amount of glucose in the blood. When you eat, your body breaks down carbohydrates into glucose, which then enters the bloodstream.
Here, insulin comes into play by allowing your cells to absorb this glucose for energy. Any excess glucose is stored in the liver for later use.
In a healthy individual, insulin levels rise and fall in response to food intake, keeping blood sugar levels stable throughout the day.
For someone with type 1 diabetes, this process does not happen because the pancreas has stopped producing insulin. Underdeveloped pancreas lead to neonatal diabetes with most patients not even knowing about this.
The result?
Blood sugar levels rise unchecked, which can cause severe short-term and long-term complications if not managed.
What Happens in Type 1 Diabetes?
So, what exactly happens in type 1 diabetes?
In this autoimmune condition, the body’s immune system mistakenly attacks the beta cells in the pancreas, the very cells responsible for insulin production.
The immune system views these cells as foreign invaders and systematically destroys them, leading to diabetes no insulin is produced.
As a result, someone with type 1 diabetes must manually regulate their blood sugar using insulin injections or an insulin pump.
Unlike type 2 diabetes, which can sometimes be managed with diet or natural methods (such as eating chromium for blood sugar control) and exercise (such as jogging safely to treat type 2 diabetes), type 1 diabetes is insulin-dependent.
There is no escaping the fact that, for these individuals, the pancreas not producing insulin leads to a lifetime of insulin therapy.
Why Does the Pancreas Stop Producing Insulin?
The exact reason why the immune system targets the beta cells in type 1 diabetes is still a subject of ongoing research.
Genetic factors play a big role, as does exposure to certain environmental triggers like viruses. The loss of insulin production is gradual, and by the time someone is diagnosed, up to 90% of their beta cells may already be destroyed.
Interestingly, some people with newly diagnosed type 1 diabetes may still have a small amount of insulin production.
This is referred to as the “honeymoon phase,” where the type 1 diabetes still producing insulin but at insufficient levels to regulate blood sugar.
However, this phase doesn’t last long, and soon, insulin production ceases entirely.
Daily Life with Type 1 Diabetes
Living with type 1 diabetes means keeping a constant eye on your blood sugar levels and calculating how much insulin your body needs to function properly.
Take, for example, a simple daily activity like having breakfast. A person without diabetes does not think twice about the carbs in their cereal or the sugar in their coffee.
But for someone with type 1 diabetes, every meal requires careful planning.
Imagine having to calculate how many grams of carbs are in your toast, measure your blood sugar, and then figure out how much insulin to inject—all before taking a single bite.
Miss the mark on either side and you could experience low blood sugar (hypoglycemia) or high blood sugar (hyperglycemia), both of which can be dangerous.
Scientific Studies on Insulin and T1D
There is no shortage of research on insulin and its role in type 1 diabetes.
A study published in the Journal of Clinical Endocrinology & Metabolism found that maintaining near-normal blood glucose levels through insulin therapy significantly reduces the risk of complications associated with type 1 diabetes, such as neuropathy and retinopathy.
This highlights the importance of insulin in managing the condition.
Another study in Diabetes Care emphasized the crucial role of early insulin intervention to preserve any remaining beta-cell function during the initial diagnosis.
While the type 1 diabetes produce insulin phase might be short-lived, preserving even a small amount of insulin production can make diabetes management easier in the early stages.
The Role of Insulin in Type 1 Diabetes – My Conclusive Analysis:
In conclusion, the role of insulin in type 1 diabetes is not just essential—it is life-saving.
Without insulin, the body simply cannot regulate blood sugar, leading to a wide range of dangerous complications.
Insulin therapy allows individuals with type 1 diabetes to mimic the natural insulin function, although it requires constant vigilance and adjustment.
To answer the question, “What is the role of insulin hormone in type 1 diabetes?”—it is the key to survival.
The body’s inability to produce insulin due to an autoimmune attack on the beta cells of the pancreas leaves those with type 1 diabetes dependent on external sources such as insulin injections to control blood sugar levels.
This hormone is not just about controlling blood sugar, it is about sustaining life and preventing the devastating effects of unmanaged diabetes.
While there is currently no cure for type 1 diabetes, try herbs that lower blood sugar fast. Advancements in insulin delivery and management have come a long way, making it possible for people to live full, active lives despite the condition.
The key lies in understanding insulin’s role and using it effectively to manage the complexities of type 1 diabetes.
References: