What Is the Difference Between LADA Type 1 and Type 2 Diabetes?
- admin
- February 4, 2025
- 5:50 pm
- No Comments
Diabetes is a chronic condition that affects millions of people worldwide, but not all diabetes is the same.
While Type 1 and Type 2 diabetes are well-known, there is a lesser-known form called Latent Autoimmune Diabetes in Adults (LADA).
This condition shares characteristics of both Type 1 and Type 2 diabetes, often leading to misdiagnosis.
Understanding the differences between LADA and Type 1 diabetes as well as the differences between LADA and Type 2 diabetes is crucial for accurate diagnosis and effective treatment.
This article provides an in-depth comparison of LADA, Type 1, and Type 2 diabetes, covering their causes, symptoms, progression, diagnosis, and treatment.
Whether you or a loved one has been diagnosed with diabetes or you are seeking more knowledge, this guide will help you understand these distinct types of diabetes.
In the Article:
- Understanding Diabetes: An Overview
- What Is Type 1 Diabetes?
- What Is Type 2 Diabetes?
- What Is LADA Diabetes?
- Key Differences Between LADA, Type 1, and Type 2 Diabetes
- Diagnosis and Misdiagnosis of LADA
- Progression of LADA Diabetes Compared to Other Types
- Treatment Options for LADA Diabetes
- Risk Factors for Developing LADA
- Conclusion
Understanding Diabetes: An Overview
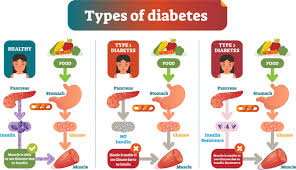
Diabetes mellitus is a metabolic disorder that leads to high blood sugar levels due to insulin-related issues.
Insulin, a hormone produced by the pancreas, plays a crucial role in regulating glucose metabolism by allowing cells to absorb and utilize glucose for energy.
When insulin production is impaired or when the body’s cells develop insulin resistance, blood sugar levels rise, leading to hyperglycemia.
According to a study published in the Journal of Clinical Endocrinology & Metabolism, diabetes affects over 400 million people globally, making it a significant public health concern.
Type 1 diabetes is an autoimmune condition where the immune system destroys insulin-producing beta cells, while Type 2 diabetes is often associated with obesity and lifestyle factors.
Latent Autoimmune Diabetes in Adults (LADA) shares characteristics of both Type 1 and Type 2 diabetes, progressing more slowly than Type 1 but still requiring insulin therapy over time.
Each type has distinct pathophysiology and treatment strategies, making early and accurate diagnosis essential for effective management.
What Is Type 1 Diabetes?
Type 1 diabetes is an autoimmune condition where the body’s immune system mistakenly attacks insulin-producing beta cells in the pancreas, leading to a severe reduction or complete loss of insulin production.
Without insulin, the body cannot properly regulate blood sugar levels, resulting in hyperglycemia.
Since insulin is essential for glucose uptake into cells, individuals with Type 1 diabetes require lifelong insulin therapy to maintain normal blood sugar levels and prevent complications.
Symptoms of Type 1 diabetes often appear suddenly and can include excessive thirst, frequent urination, unexplained weight loss, extreme fatigue, and blurred vision.
In some cases, individuals may also experience increased hunger, mood changes, or slow-healing wounds. This type of diabetes is most commonly diagnosed in children, teenagers, and young adults, although it can develop at any age.
The autoimmune diabetes in adults category includes LADA, which progresses differently from traditional Type 1 diabetes, typically presenting a slower onset and initially requiring non-insulin treatments before progressing to full insulin dependence.
What Is Type 2 Diabetes?
Type 2 diabetes is the most common form of diabetes, primarily caused by insulin resistance. In this condition, the body’s cells do not respond properly to insulin, leading to elevated blood sugar levels. Over time, the pancreas struggles to produce enough insulin to maintain normal glucose levels.
Type 2 diabetes is often associated with obesity, poor diet, and a sedentary lifestyle. Symptoms develop gradually and can include increased thirst, frequent urination, fatigue, slow wound healing, and blurred vision.
Unlike Type 1 diabetes, many people with Type 2 diabetes can manage their condition with lifestyle changes, oral medications, and sometimes insulin therapy. However, misdiagnosis of LADA as Type 2 diabetes is common due to the gradual onset of symptoms in both conditions.
What Is LADA Diabetes?
LADA, or Latent Autoimmune Diabetes in Adults, is a slow-progressing form of autoimmune diabetes that shares features of both Type 1 and Type 2 diabetes. It is often diagnosed in adults over 30 who initially do not require insulin.
One of the biggest challenges with diagnosis of LADA diabetes is that it is frequently mistaken for Type 2 diabetes. Unlike Type 2 diabetes, LADA involves autoimmune destruction of beta cells, similar to Type 1 diabetes, but this process occurs at a much slower rate.
Common symptoms of Latent Autoimmune Diabetes in Adults include frequent urination, excessive thirst, and unexplained weight loss. However, because insulin dependency develops gradually, many people with LADA are initially prescribed oral medications before transitioning to insulin therapy.
Key Differences Between LADA, Type 1, and Type 2 Diabetes
Understanding the differences between LADA and Type 1 diabetes, as well as the differences between LADA and Type 2 diabetes, is essential for ensuring accurate diagnosis and proper treatment. While all three conditions affect blood sugar regulation, they differ significantly in their causes, progression, and treatment approaches.
Below are the key differences:
- Age of Onset: Type 1 diabetes is typically diagnosed in children and young adults, often before the age of 30. Type 2 diabetes generally develops later in life, though increasing obesity rates have led to diagnoses in younger individuals. LADA, however, occurs in adults over 30 and progresses more slowly than Type 1.
- Autoimmune Nature: Both LADA and Type 1 diabetes are autoimmune diseases, meaning the immune system mistakenly attacks insulin-producing beta cells in the pancreas. Type 2 diabetes, on the other hand, is primarily caused by insulin resistance and is not considered an autoimmune disorder.
- Progression: Type 1 diabetes has a rapid onset, often requiring immediate insulin therapy due to the swift destruction of beta cells. LADA develops more gradually, sometimes taking years before insulin dependency occurs. Type 2 diabetes progresses slowly and can often be managed with lifestyle changes and oral medications for an extended period.
- Initial Treatment: People with Type 2 diabetes and LADA may start treatment with oral medications such as metformin. However, while Type 2 diabetes patients can manage their condition without insulin for years, LADA patients will eventually require insulin therapy as beta cell function declines.
- Family History and Risk Factors: Type 2 diabetes has a stronger link to obesity and lifestyle factors, whereas LADA and Type 1 diabetes are more closely associated with genetic reasons and autoimmune components. Individuals with a family history of autoimmune diseases are at higher risk for developing LADA or Type 1 diabetes.
- C-Peptide Levels: C-peptide, a marker of insulin production, is low in both LADA and Type 1 diabetes due to beta cell destruction. In Type 2 diabetes, C-peptide levels are usually normal or high because the pancreas is still producing insulin, but the body is resistant to its effects.
Recognizing these differences is crucial for determining the most appropriate treatment plan. Misdiagnosis, especially of LADA as Type 2 diabetes, can lead to ineffective treatments and long-term complications.
Diagnosis and Misdiagnosis of LADA
Since LADA develops gradually, it is often misdiagnosed as Type 2 diabetes, particularly in its early stages when insulin production is still sufficient to manage blood sugar levels.
However, unlike Type 2 diabetes, LADA is an autoimmune condition, meaning the body’s immune system progressively destroys insulin-producing beta cells.
The diagnosis of LADA diabetes involves testing for specific autoantibodies, such as glutamic acid decarboxylase antibodies (GADAs), which are found in both LADA and Type 1 diabetes but are absent in Type 2 diabetes.
Due to the frequent misdiagnosis of LADA as Type 2 diabetes, many patients are initially prescribed oral diabetes medications, such as metformin or sulfonylureas, which do not address the underlying autoimmune process.
Over time, as beta-cell function declines, blood sugar control worsens, eventually necessitating insulin therapy. Early and accurate diagnosis is crucial for proper treatment and management of LADA.
Progression of LADA Diabetes Compared to Other Types
The progression of LADA diabetes follows a unique pattern, developing more slowly than Type 1 diabetes but more rapidly than Type 2 diabetes in terms of beta-cell destruction.
While Type 1 diabetes leads to a quick and almost complete loss of insulin production, LADA progresses over several months or years before insulin dependency becomes necessary.
This gradual decline can initially make it appear similar to Type 2 diabetes, leading to misdiagnosis and inappropriate treatment.
As the immune system continues attacking insulin-producing beta cells, blood sugar levels become increasingly difficult to manage with oral medications alone.
Over time, LADA patients will require insulin therapy to maintain stable blood glucose levels, similar to those with Type 1 diabetes. Proper diagnosis and timely intervention with insulin can help slow beta-cell destruction and improve long-term outcomes for individuals with LADA.
Treatment Options for LADA Diabetes
The treatment options for LADA diabetes depend on how much insulin the body is still producing. Initially, lifestyle changes and oral medications may be used, but insulin therapy will eventually become necessary.
- Early Intervention: Starting insulin therapy early may help preserve remaining beta-cell function.
- Diet and Exercise: A balanced diet and regular physical activity can help manage blood sugar levels.
- Blood Sugar Monitoring: Regular glucose monitoring using glucometers is essential to adjust treatment as needed.
Risk Factors for Developing LADA
While the risk factors for developing LADA are not entirely understood, research suggests that a combination of genetic predisposition, family history of autoimmune diseases, and environmental triggers contribute to its onset.
According to a study published in Diabetes Care, individuals with certain HLA gene variants, commonly associated with Type 1 diabetes, have a higher risk of developing LADA.
Environmental factors such as viral infections and diet may also influence disease progression.
People diagnosed with Type 2 diabetes who are not overweight and struggle to manage blood sugar levels with oral medications should be tested for LADA to ensure appropriate treatment and prevent complications.
Conclusion
LADA, Type 1, and Type 2 diabetes share some similarities, but they differ significantly in their causes, progression, and treatment approaches.
Type 1 diabetes results from a rapid autoimmune attack on insulin-producing beta cells, requiring immediate insulin therapy. Type 2 diabetes, on the other hand, is primarily driven by insulin resistance and can often be managed with lifestyle changes and oral medications.
LADA falls between these two, with a slower autoimmune progression, leading to insulin dependence over time.
Recognizing the differences between these conditions is crucial for accurate diagnosis and effective treatment. Many individuals with LADA are initially misdiagnosed as having Type 2 diabetes, delaying the appropriate treatment.
Early detection through autoantibody testing can help ensure better long-term blood sugar control and reduce complications.
References: