How Cholesterol Affects Blood Sugar Control in Type 2 Diabetes?
- admin
- October 26, 2024
- 1:23 pm
- No Comments
Ah, the classic clash of cholesterol and blood sugar—it is more intense than any reality TV drama.
If you are dealing with type 2 diabetes, managing blood sugar levels is already a tricky dance.
But throw cholesterol into the mix, and things get even more complicated.
In this article, we are going to dive deep into how cholesterol impacts blood sugar control, what science says about it, and what you can do to manage both effectively.
Article Index
- Introduction to Cholesterol and Diabetes
- The Role of Cholesterol in Blood Sugar Regulation
- The Science Behind High Cholesterol and Insulin Resistance
- Real-Life Scenarios: How Cholesterol Levels Affect Diabetic Patients
- Cholesterol Management Strategies for Type 2 Diabetics
- The Impact of Medications: Statins, GLP-1 Cholesterol, and Others
- Conclusion: The Balancing Act of Cholesterol and Blood Sugar
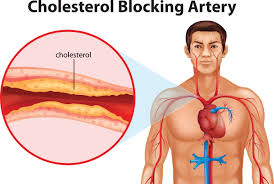
Introduction to Cholesterol and Diabetes
Let us start with the basics: cholesterol is not the villain you might think it is.
It is a waxy substance your body needs to build cells. However, in type 2 diabetes, the balance between “good” (HDL) and “bad” (LDL) cholesterol often gets out of whack.
This imbalance, combined with elevated blood glucose levels, sets the stage for what’s called diabetic dyslipidemia—a fancy way of saying cholesterol levels are all over the place when diabetes is present.
The Role of Cholesterol in Blood Sugar Regulation
Believe it or not, cholesterol plays a critical role in blood sugar management. Studies have shown that HDL cholesterol has a beneficial effect on insulin secretion and glucose uptake in muscles.
It acts like the superhero that gets insulin to do its job effectively.
However, when HDL is low and LDL is high, which is common in type 2 diabetes, this superhero power diminishes, making it harder to control blood sugar levels.
The Science Behind High Cholesterol and Insulin Resistance
Okay, here is where things get technical but bear with me—it is crucial.
Free fatty acids (FFAs), which are byproducts of high LDL cholesterol, interfere with insulin signaling.
A study in Diabetes Care explains how FFAs trigger pathways that reduce insulin sensitivity, making it harder for your body to lower blood sugar levels.
This leads to a vicious cycle: the more insulin-resistant your body becomes, the higher your blood sugar and LDL cholesterol levels go
But why does this happen?
The American Diabetes Association points to the accumulation of diacylglycerol (DAG) in muscle cells when FFA levels are high. DAG activates protein kinase C (PKC), an enzyme that disrupts the insulin receptor pathway.
This not only makes insulin less effective but also raises blood sugar levels.
Real-Life Scenarios: How Cholesterol Levels Affect Diabetic Patients
Let us look at Diana, a 55-year-old woman with type 2 diabetes and high LDL cholesterol (or “type 2 diabetes high cholesterol”).
Diana struggles to maintain her blood sugar levels despite following a strict diet and exercise regimen.
Her doctor explains that her elevated LDL cholesterol and low HDL cholesterol are making it harder for her insulin to work effectively.
In fact, LDL cholesterol molecules in people with diabetes tend to be smaller and denser, increasing their likelihood of contributing to cardiovascular issues and worsening insulin resistance
Cholesterol Management Strategies for Type 2 Diabetics
To manage both cholesterol and blood sugar levels effectively, it is crucial to adopt a multifaceted approach:
- Dietary Changes: Reducing saturated fats and increasing fiber intake can significantly lower LDL cholesterol. The National Cholesterol Education Program recommends keeping saturated fats to less than 7% of daily calories for people with diabetes.
- Exercise: Regular physical activity can help boost HDL (“good”) cholesterol levels while also improving insulin sensitivity. The American Heart Association emphasizes that combining aerobic exercises with resistance training is particularly effective for type 2 diabetics.
- Weight Management: Losing even 5-10% of body weight can significantly improve cholesterol and glucose levels, according to studies published by the UK Prospective Diabetes Study (UKPDS).
The Impact of Medications: Statins, GLP-1 Cholesterol, and Others
When lifestyle changes are not enough, medications come into play.
Statins, such as atorvastatin and simvastatin, are often prescribed to manage high cholesterol in diabetics. Research from the Heart Protection Study shows that statin use can reduce cardiovascular risks even when LDL cholesterol levels are not excessively high.
However, there is a catch: some studies suggest that statins may slightly increase blood glucose levels, raising concerns about type 2 diabetes and high cholesterol management.
On the flip side, GLP-1 cholesterol medications like liraglutide have shown promise in improving both blood sugar and cholesterol levels simultaneously.
They work by increasing insulin secretion and lowering triglycerides, making them a useful tool for those struggling with “dm 2 w hyperlipidemia.” Still, these medications should be used under medical supervision as their effects can vary.
For some, ezetimibe (Zetia) is another option.
This medication helps lower cholesterol absorption in the intestines, making it a good choice for people who have type 2 diabetes high blood pressure and high cholesterol.
Studies suggest that combining Zetia with statins could be particularly effective for managing cholesterol levels for diabetes type 2 patients.
The Balancing Act of Cholesterol and Blood Sugar
Cholesterol and blood sugar levels are like dance partners in the body—they need to be in sync for everything to work smoothly.
For those managing type 2 diabetes, keeping cholesterol levels in check is not just about heart health; it is about improving insulin sensitivity and blood sugar control.
The “target cholesterol for type 2 diabetes NICE” guidelines suggest that LDL levels should be below 100 mg/dL, with an optimal target of less than 70 mg/dL for those at high cardiovascular risk.
To sum it all up, if you have type 2 diabetes and are battling high cholesterol, focus on a comprehensive approach: diet, exercise, weight management, and medication if necessary.
Talk to your doctor about which strategy is best for you, as achieving the right balance between cholesterol and glucose levels can be the key to a healthier, more vibrant life.
References: