What is Beta-Cell Failure in the Context of LADA?
- admin
- February 6, 2025
- 6:54 am
- No Comments
Latent Autoimmune Diabetes in Adults (LADA) is a unique form of diabetes that straddles the characteristics of both Type 1 and Type 2 diabetes.
LADA is very different from Type 1 and Type 2 diabetes.
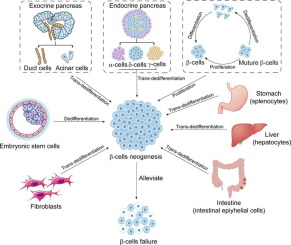
One of the critical aspects of LADA is the progressive failure of beta cells in the pancreas, which are responsible for insulin production.
This article delves into the definition of beta-cell failure within the context of LADA, exploring its causes, progression, and implications for treatment.
Article Index
- Overview of LADA
- Role of Beta Cells in Glucose Regulation
- Mechanisms Leading to Beta-Cell Failure in LADA
- Comparison of Beta-Cell Failure in LADA, Type 1, and Type 2 Diabetes
- Diagnosis of Beta-Cell Dysfunction in LADA
- Implications of Beta-Cell Failure for Treatment Strategies
- FAQs on Beta-Cell Failure in LADA
- Conclusion
Overview of LADA
LADA is often referred to as Type 1.5 diabetes because it exhibits features of both Type 1 and Type 2 diabetes.
Typically diagnosed in adults over the age of 30, LADA is characterized by the presence of autoantibodies against pancreatic islet cells, indicating an autoimmune component similar to Type 1 diabetes.
However, unlike the rapid onset of Type 1 diabetes, LADA progresses more slowly, and patients may not require insulin therapy immediately upon diagnosis.
This gradual progression often leads to an initial misdiagnosis of Type 2 diabetes.
Role of Beta Cells in Glucose Regulation
Beta cells, located in the islets of Langerhans within the pancreas, are crucial for maintaining blood glucose levels by producing and releasing insulin.
Insulin is a hormone that regulates glucose metabolism by facilitating the uptake of glucose into muscle, liver, and fat cells, where it is either used for energy or stored for future use.
When blood glucose levels rise, such as after eating, beta cells respond by secreting insulin to lower blood sugar levels and maintain homeostasis.
The proper functioning of beta cells is essential for metabolic balance, and any disruption in their ability to produce insulin can lead to chronic hyperglycemia, a defining characteristic of diabetes. In conditions such as Type 1 diabetes and Latent Autoimmune Diabetes in Adults (LADA), an autoimmune response gradually destroys beta cells, reducing insulin secretion.
In Type 2 diabetes, prolonged insulin resistance causes beta-cell dysfunction, leading to insufficient insulin production over time and worsening glucose control.
Mechanisms Leading to Beta-Cell Failure in LADA
In LADA, beta-cell failure is primarily driven by an autoimmune response. The body’s immune system mistakenly targets and destroys beta cells, leading to a gradual decline in insulin production.
Research indicates that both innate and adaptive immune mechanisms are involved. For instance, macrophages infiltrate pancreatic islets and produce pro-inflammatory cytokines like interleukin-1β (IL-1β), which contribute to beta-cell apoptosis.
Additionally, autoantibodies such as glutamic acid decarboxylase antibodies (GADAs) are commonly present in LADA patients, serving as markers of the autoimmune attack on beta cells.
Comparison of Beta-Cell Failure in LADA, Type 1, and Type 2 Diabetes
While beta-cell failure occurs in both Type 1 and Type 2 diabetes, the underlying mechanisms and progression rates differ.
In Type 1 diabetes, there is a rapid and complete autoimmune destruction of beta cells, leading to an abrupt cessation of insulin production.
Over here autoimmunity and LADA seem to have an uncanny connection which is often misdiagnosed.
Conversely, in Type 2 diabetes, beta-cell dysfunction is primarily due to insulin resistance and metabolic stress, with beta cells gradually losing their ability to compensate for increased insulin demand.
LADA occupies an intermediate position. The autoimmune destruction of beta cells is slower than in Type 1 diabetes, allowing for a longer period before insulin dependence becomes necessary.
However, the progression is more rapid than in Type 2 diabetes, with studies showing that LADA patients with multiple islet autoantibodies often develop significant beta-cell failure within five years of diagnosis.
>>> Want to Learn How I “Treated My Diabetes Naturally” at Home??? Click Here to Find Out! <<<
Diagnosis of Beta-Cell Dysfunction in LADA
Accurate diagnosis of beta-cell dysfunction in LADA involves several approaches:
- Autoantibody Testing: Detecting the presence of autoantibodies such as GADAs is crucial for identifying the autoimmune component of LADA. These autoantibodies are typically absent in Type 2 diabetes patients.
- C-Peptide Measurement: C-peptide levels serve as a marker of endogenous insulin production. In LADA, C-peptide levels are generally lower than in Type 2 diabetes, reflecting impaired beta-cell function.
- Genetic Testing: While not routinely performed, genetic testing can identify specific HLA genotypes associated with increased susceptibility to autoimmune diabetes, providing further evidence supporting a LADA diagnosis.
Implications of Beta-Cell Failure for Treatment Strategies
Understanding the trajectory of beta-cell failure in LADA is crucial for developing effective treatment strategies that prevent rapid disease progression and improve long-term outcomes.
Since LADA is an autoimmune condition, early initiation of insulin therapy may help preserve residual beta-cell function and slow the decline in insulin production.
Research suggests that starting insulin treatment earlier in the disease course reduces the burden on beta cells, potentially delaying full insulin dependence.
Some studies also indicate that combining insulin with immunomodulatory agents, such as dipeptidyl peptidase-4 (DPP-4) inhibitors, may provide additional protection for beta cells, though more clinical trials are needed to confirm this approach.
Lifestyle interventions, including a balanced diet and regular physical activity, are essential for optimizing blood sugar control.
However, unlike Type 2 diabetes, where oral hypoglycemic agents like metformin can be effective for years, LADA patients experience a progressive decline in insulin production, making oral medications insufficient as a long-term treatment.
FAQs on Beta-Cell Failure in LADA
Q-1: How does beta-cell failure in LADA differ mechanistically from that in classic type 1 diabetes?
A-1: In LADA (Latent Autoimmune Diabetes in Adults), beta-cell failure occurs through a slower, more gradual autoimmune destruction compared to the rapid beta-cell loss seen in classic type 1 diabetes. This slower progression allows some residual insulin production for months or years, making the clinical onset less acute but ultimately leading to similar beta-cell depletion.
Q-2: What role does immune-mediated inflammation play specifically in beta-cell failure within LADA?
A-2: Immune-mediated inflammation in LADA targets pancreatic beta cells through autoreactive T cells and autoantibodies, causing chronic low-grade inflammation. This persistent immune attack not only destroys beta cells over time but also disrupts their function before outright cell death, contributing to a progressive decline in insulin secretion unique to LADA’s pathophysiology.
Q-3: Can beta-cell failure in LADA be partially reversible or halted during early stages?
A-3: Emerging evidence suggests that early intervention in LADA with immune-modulating therapies or tight glycemic control may slow or partially preserve beta-cell function. While complete reversal is unlikely, stabilizing beta-cell health during the initial phase could delay insulin dependency and improve long-term outcomes.
Q-4: How does beta-cell failure impact the clinical management strategies specific to LADA patients?
A-4: Because beta-cell failure in LADA is gradual, initial treatment often starts with oral hypoglycemics rather than immediate insulin. However, clinicians must closely monitor beta-cell function markers and autoantibody levels to anticipate insulin initiation as beta-cell failure progresses, tailoring therapy to preserve residual insulin production as long as possible.
Q-5: What biomarkers are most indicative of ongoing beta-cell failure in LADA compared to other diabetes types?
A-5: In LADA, the presence of autoantibodies such as GAD65 and IA-2, combined with declining C-peptide levels, uniquely signals ongoing beta-cell failure. These markers help differentiate LADA from type 2 diabetes, where autoimmunity is absent, and guide clinicians in tracking beta-cell decline.
Q-6: How does the pattern of beta-cell failure in LADA influence the risk of diabetes-related complications?
A-6: The gradual beta-cell failure in LADA leads to fluctuating insulin levels, which can cause variable blood glucose control and increase the risk of both hyperglycemia and hypoglycemia. This instability heightens the risk for microvascular complications and necessitates vigilant monitoring and tailored treatment to mitigate long-term damage.
These FAQs provide nuanced insights into the unique nature of beta-cell failure in LADA, offering clarity for patients and healthcare providers navigating this complex diabetes subtype.
Conclusion
Beta-cell failure in LADA is marked by a gradual autoimmune-mediated decline in insulin production, setting it apart from the rapid beta-cell destruction observed in Type 1 diabetes and the insulin resistance-driven dysfunction in Type 2 diabetes.
This slow progression often leads to an initial misdiagnosis of Type 2 diabetes, delaying the initiation of proper treatment.
According to research published in Diabetes Care, individuals with LADA experience a progressive loss of insulin secretion, with approximately 50% requiring insulin therapy within five years of diagnosis.
Unlike Type 2 diabetes, where beta-cell dysfunction is influenced by metabolic stress and insulin resistance, LADA involves an autoimmune attack that targets beta cells, leading to eventual insulin deficiency.
Recognizing this distinct trajectory is crucial for ensuring an accurate diagnosis and implementing timely interventions.
Studies suggest that early insulin therapy may help preserve residual beta-cell function and slow disease progression.
Proper management, including lifestyle modifications and careful monitoring, can optimize blood glucose control and improve long-term outcomes for LADA patients.
References: