- admin
- November 9, 2024
- 12:17 pm
- No Comments
How Pancreatic Hormone Imbalance Leads to Type 3c Diabetes?
When we think of diabetes, it is often the big two—Type 1 and Type 2—that dominate the conversation.
But there is another player in the game:
Type 3c diabetes.
This form of diabetes is not just a side effect of bad luck or genetics; it is often tied to a very specific culprit—your pancreas and its out-of-whack hormones.
In this article, BestDietarySupplementforDabetics researchers would take a deep dive into how pancreatic hormone imbalances lead to type 3c diabetes.
Spoiler alert: it is a fascinating (and a little sneaky) process.
Here is what we’ll cover:
- What is Type 3c Diabetes?
- The Role of the Pancreas in Hormone Regulation
- Key Pancreatic Hormones and Their Function
- How Hormonal Imbalance Sets the Stage for Type 3c Diabetes
- Real-Life Example: John’s Journey to a Type 3c Diagnosis
- Scientific Evidence Linking Hormone Imbalance to Type 3c Diabetes
- FAQs on Type 3c Diabetes & Pancreatic Hormonal Imbalance
- The Long-Term Impact of Pancreatic Dysfunction
Let us roll up our sleeves and get into the nitty-gritty of how your pancreas holds the keys to your metabolic destiny.
What is Type 3c Diabetes?
Type 3c diabetes, also called pancreatogenic diabetes, occurs when pancreatic damage leads to dysfunction in both the endocrine (hormone-producing) and exocrine (enzyme-producing) parts of the pancreas.
This is not your typical diabetes story of insulin resistance or autoimmune destruction—it is a condition that stems from diseases, surgeries, or injuries affecting the pancreas.
Patients with type 3c diabetes often struggle with both blood sugar regulation and digestion, thanks to a double whammy of hormone imbalance and enzyme insufficiency.
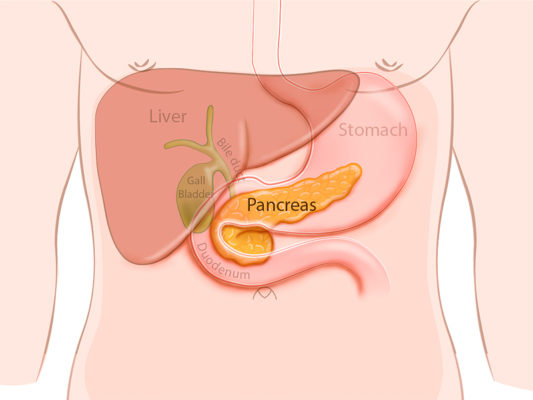
The Role of the Pancreas in Hormone Regulation
Your pancreas is a multitasking marvel, quietly operating behind your stomach and playing a critical role in maintaining your body’s equilibrium.
This small but mighty organ manages two essential systems that keep your body running smoothly:
1. Endocrine Function:
The pancreas produces key hormones like insulin, glucagon, and somatostatin, which work together to regulate blood sugar levels.
Insulin helps lower blood sugar by enabling cells to absorb glucose, while glucagon raises blood sugar when it dips too low.
Somatostatin acts as a regulator, preventing these hormones from getting out of control.
This intricate balancing act ensures your body has the energy it needs throughout the day.
2. Exocrine Function:
Beyond hormones, the pancreas also produces digestive enzymes like amylase, lipase, and protease.
These enzymes are essential for breaking down carbohydrates, fats, and proteins in your gut, ensuring your body can absorb the nutrients it requires.
When the pancreas is damaged—due to conditions like pancreatitis, tumors, or surgery—it disrupts both endocrine and exocrine functions.
The first sign of trouble is often an imbalance in pancreatic hormones.
Without sufficient insulin or with unchecked glucagon, blood sugar regulation falters, leading to hyperglycemia.
This hormonal chaos, coupled with enzyme deficiencies, is the foundation of type 3c diabetes.
Understanding the dual roles of the pancreas highlights how its dysfunction creates a domino effect, leading to complex metabolic issues that require targeted care and management.
Key Pancreatic Hormones and Their Function
Let’s meet the key players in the delicate hormonal balancing act performed by your pancreas.
These hormones work together like a well-rehearsed orchestra to regulate blood sugar levels and maintain overall metabolic harmony:
- Insulin: Often referred to as the hero of glucose regulation, insulin helps cells absorb sugar from the bloodstream, providing energy to tissues and keeping blood sugar levels in check. Without it, sugar would remain in your blood, leading to hyperglycemia.
- Glucagon: This hormone serves as insulin’s counterweight, stepping in when blood sugar levels drop too low. It signals the liver to release stored glucose, ensuring your body has a steady energy supply, especially between meals.
- Somatostatin: Known as the peacekeeper, somatostatin ensures that neither insulin nor glucagon goes rogue. By regulating the release of these hormones, it maintains a fine balance that prevents blood sugar spikes or crashes.
- Pancreatic Polypeptide (PP): This lesser-known hormone plays a role in regulating digestive processes and appetite control, adding another layer of complexity to the metabolic system.
When these hormones fall out of sync—whether due to pancreatic damage, inflammation, or disease—your body’s ability to regulate blood sugar is compromised.
The result is a cascade of metabolic dysfunctions, which can pave the way for type 3c diabetes, a condition rooted in both hormonal imbalance and digestive disruption.
How Hormonal Imbalance Sets the Stage for Type 3c Diabetes?
Damage to the pancreas throws its finely tuned hormonal orchestra into complete disarray, leading to a cascade of metabolic dysfunctions that can pave the way for type 3c diabetes.
Here is how the chaos unfolds:
Insufficient Insulin Production:
Insulin, the star player in blood sugar regulation, is often the first casualty when the pancreas is damaged.
This hormone enables cells to absorb glucose from the bloodstream, keeping sugar levels stable.
When insulin production falters, glucose accumulates in the blood, creating the hallmark hyperglycemia associated with diabetes.
Over time, this can lead to significant metabolic complications and strain on organs like the kidneys and heart.
Excess Glucagon:
As insulin production dwindles, glucagon—a hormone that raises blood sugar—steps into the spotlight unchecked.
Its job is to signal the liver to release stored glucose during fasting states, but without the balancing effect of insulin, glucagon’s activity goes into overdrive.
The result?
The liver releases an excess of glucose, worsening already elevated blood sugar levels.
Disrupted Balance of Somatostatin and Pancreatic Polypeptide (PP)
Often overshadowed by insulin and glucagon, somatostatin and pancreatic polypeptide are crucial for maintaining hormonal balance.
Somatostatin prevents runaway insulin and glucagon activity, while PP regulates digestive processes and appetite. Pancreatic damage disrupts their production, further destabilizing metabolic equilibrium.
Together, these hormonal imbalances create a domino effect, leading to the development and progression of type 3c diabetes—a condition that underscores the intricate interplay of pancreatic hormones.
Real-Life Example: John’s Journey to a Type 3c Diagnosis
John, a 45-year-old architect, began experiencing unexplained weight loss, fatigue, and frequent trips to the bathroom.
Partial pancreatectomy triggering type 3c diabetes is what was explained to her by her medical supervisor.
Initially, doctors suspected type 2 diabetes, but a deeper dive into his history revealed chronic pancreatitis from years of untreated gallstones.
His tests showed low insulin levels, elevated glucagon, and digestive enzyme deficiencies.
The culprit?
Pancreatic damage had thrown his hormones into disarray, leading to type 3c diabetes.
John’s story highlights the importance of identifying the root cause of diabetes symptoms, particularly when pancreatic damage is involved.
Scientific Evidence Linking Hormone Imbalance to Type 3c Diabetes
Science has been shedding light on the connection between pancreatic dysfunction and type 3c diabetes:
- “Pancreatic Endocrine Dysfunction in Chronic Pancreatitis” (Clinical Gastroenterology and Hepatology, 2020): This study found that 40-70% of patients with chronic pancreatitis develop type 3c diabetes due to impaired hormone production.
- “Hormonal Imbalance in Pancreatogenic Diabetes” (Diabetes Care, 2019): Researchers noted that reduced insulin and dysregulated glucagon levels are central to the development of type 3c diabetes.
- “Pancreatic Hormone Dynamics Post-Surgery” (World Journal of Surgery, 2021): Highlighted how partial pancreas removal leads to hormonal imbalance, significantly increasing the risk of type 3c diabetes.
The Long-Term Impact of Pancreatic Dysfunction
Left unmanaged, the hormonal imbalances in type 3c diabetes set the stage for a host of severe complications, many of which go beyond just blood sugar control.
Here are the key issues that can arise:
1. Hyperglycemia:
Prolonged high blood sugar is a hallmark of diabetes, and in type 3c diabetes, it often goes unchecked due to insufficient insulin production and excessive glucagon activity.
This chronic hyperglycemia damages nerves (leading to neuropathy), blood vessels (increasing the risk of poor circulation and wounds that don’t heal), and vital organs such as the kidneys and eyes.
Over time, these effects significantly diminish quality of life.
2. Digestive Issues:
The pancreas does not just regulate hormones—it also produces digestive enzymes.
In type 3c diabetes, pancreatic enzyme insufficiency leads to malnutrition and weight loss, as the body struggles to break down and absorb nutrients.
Patients often experience digestive issues such as bloating, diarrhea, and fatigue as a result.
3. Increased Cardiovascular Risk:
Poorly controlled blood sugar significantly raises the risk of heart disease and stroke.
The combination of chronic inflammation, high glucose levels, and damaged blood vessels creates a perfect storm for cardiovascular complications in type 3c diabetes.
4. Chronic Pain:
Pancreatic inflammation is a common underlying condition in type 3c diabetes and can result in persistent abdominal pain.
This pain often becomes a long-term issue, further reducing the patient’s quality of life.
A study in The Lancet Endocrinology (2022) revealed that patients with type 3c diabetes have a 30% higher risk of complications compared to those with type 2 diabetes, emphasizing the need for early diagnosis and tailored management.
FAQs on Type 3c Diabetes & Pancreatic Hormonal Imbalance
Q-1: How does losing both insulin and glucagon control make glucose swings in Type 3c diabetes different from Type 2?
A-1: Pancreatic damage lowers insulin from β-cells and weakens the α-cell glucagon response. That combo means bigger post-meal highs (not enough insulin) and a higher risk of fasting or post-exercise lows (poor counter-regulation). The result is wider, less predictable glucose swings than the insulin-resistant pattern typical of Type 2.
Q-2: What role does pancreatic polypeptide (PP) deficiency play in Type 3c diabetes?
A-2: PP normally helps restrain the liver’s glucose output and fine-tunes digestion. When PP is low—common with head-predominant pancreatic damage and infection—the liver tends to release more glucose despite circulating insulin. This “hepatic bias” contributes to fasting hyperglycemia even when muscle insulin sensitivity isn’t severely impaired.
Q-3: How do incretin changes link exocrine disease to endocrine dysregulation in Type 3c?
A-3: Exocrine dysfunction alters how nutrients and bile acids reach the lower gut, blunting incretin signals that usually boost meal-time insulin release. With a weaker “food → incretin → insulin” loop, post-meal insulin secretion drops and glucose peaks run higher and longer, compounding the β-cell shortfall.
Q-4: Why can Type 3c diabetes show both insulin deficiency and signs of insulin resistance at the same time?
A-4: Multiple hormones shift at once: too little insulin, too little PP to restrain hepatic glucose output, and impaired glucagon defense. The liver behaves as if it is insulin-resistant—continuing to produce glucose—while peripheral tissues may remain comparatively sensitive. Add maldigestion and irregular nutrient delivery in the liver, and the picture looks “mixed” despite clear insulinopenia.
Q-5: How does somatostatin from δ-cells fit into the hormone imbalance of Type 3c?
A-5: Somatostatin normally “dampens” both insulin and glucagon for balance. Pancreatic injury can distort this brake—either too much local inhibition further suppressing already-low insulin and glucagon, or too little modulation leaving hepatic output unchecked. Either way, δ-cell disruption removes a stabilizer from the system, intensifying both post-meal surges and vulnerability to hypoglycemia.
Understanding the Hormone-Diabetes Connection
Pancreatic hormone imbalance is more than a side effect of pancreatic damage—it is the driving force behind type 3c diabetes.
From insulin and glucagon to somatostatin and pancreatic polypeptide, each hormone plays a critical role in maintaining metabolic harmony.
When this balance is disrupted, the consequences extend beyond blood sugar regulation, affecting digestion, energy levels, and long-term health.
Recognizing and addressing these imbalances is crucial for effectively managing type 3c diabetes and improving patient outcomes.
By understanding the interplay between pancreatic hormones and diabetes, we can better navigate this complex condition.
References: