Is Sitagliptin the Hidden Risk in Diabetes Treatment?
- admin
- August 28, 2024
- 6:58 pm
- No Comments

When it comes to managing type 2 diabetes, Sitagliptin (often marketed as Januvia) is a name that frequently pops up.
It is like the popular kid in school—everyone has heard of it, and it seems like it’s always in the spotlight.
But like any popular figure, there is always more beneath the surface.
The question that needs addressing is: Is Sitagliptin the hidden risk in diabetes treatment?
Let’s dive into the nitty-gritty to uncover the truth.
Article Index:
1) What Is Sitagliptin?
2) The Benefits: Sitagliptin’s Shiny Exterior
- Convenience
- Fewer Hypoglycemic Events
- Weight Neutral
- My Opinion on these Positive Points
3) The Hidden Risks: What You Need to Know
- Pancreatitis and Pancreatic Cancer: A Brewing Controversy
- Joint Pain: A Hidden Side Effect
- Heart Failure: The Unexpected Twist
- Kidney Function: A Subtle but Serious Concern
4) The Debate: Experts Weigh In
5) The Alternatives: Is There a Safer Option?
- Metformin: The Tried and Tested
- SGLT2 Inhibitors: The New Kid on the Block
- GLP-1 Receptor Agonists: The Heavy Hitters
6) FAQs on Sitagliptin for Diabetes Management
7) Takeaway
What Is Sitagliptin?
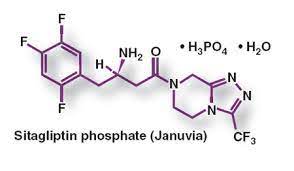
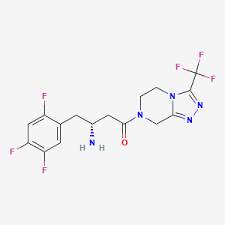
Sitagliptin belongs to a class of medications known as DPP-4 inhibitors. These drugs work by increasing the levels of incretin hormones, which help regulate blood sugar levels by increasing insulin release and decreasing glucagon levels after meals.
On the surface, this sounds like a pretty good deal, right? You take a pill, and it helps your body manage blood sugar more effectively.
But hold on—while Sitagliptin might be effective in controlling blood sugar, are there risks lurking in the background?
The Benefits: Sitagliptin’s Shiny Exterior
Before diving into the potential risks, it’s only fair to acknowledge why Sitagliptin has become a go-to for many doctors and patients.
The benefits of Sitagliptin include:
Convenience:
Sitagliptin is taken just once a day, which is a big plus for those managing diabetes.
This single daily dose means you don’t have to worry about remembering multiple pills throughout the day, making it easier to stick to your treatment plan.
The simplicity of this regimen can greatly enhance consistency, ensuring that patients stay on track with their medication and maintain better control of their blood sugar levels.
Fewer Hypoglycemic Events:
Sitagliptin stands out from many other diabetes medications because it carries a lower risk of hypoglycemia, or dangerously low blood sugar levels.
This is a significant advantage for patients, as it reduces the chances of experiencing the shaky, dizzying effects of hypoglycemia, which can be both alarming and potentially harmful.
By minimizing this risk, Sitagliptin provides a safer and more stable option for managing blood sugar levels effectively.
Weight Neutral:
One of the key benefits of Sitagliptin is that it is weight-neutral, meaning it typically does not cause weight gain—a common issue with many other diabetes medications.
For patients who are already concerned about weight management, this makes Sitagliptin an attractive option.
By avoiding unwanted weight gain, it helps patients focus on managing their blood sugar without the added worry of additional pounds.
My Opinion on these Positive Points:
From my experience, the benefits of Sitagliptin make it a really appealing choice, especially if you have had a tough time with the side effects of other medications.
It has been a relief not to deal with some of the usual issues.
But, as I have learned, when something seems almost too good to be true, it is important to dig deeper and see if there is more to the story than meets the eye.
The Hidden Risks: What You Need to Know
Here is where things get interesting—and a bit concerning.
While Sitagliptin has been praised for its benefits, some research suggests there could be risks associated with its use.
Let me break them down for you:
Pancreatitis and Pancreatic Cancer: A Brewing Controversy
One of the most alarming concerns with Sitagliptin is its potential link to pancreatitis (inflammation of the pancreas) and pancreatic cancer.
Studies have shown that DPP-4 inhibitors like Sitagliptin may increase the risk of developing pancreatitis.
A study published in JAMA Internal Medicine highlighted a significant increase in hospitalizations for acute pancreatitis among patients using Sitagliptin (Singh et al., 2013).
Even more worrisome is the potential link to pancreatic cancer. Although the data is still inconclusive, some research suggests that long-term use of Sitagliptin could elevate the risk.
A study published in Diabetes Care raised concerns about a possible association between incretin-based therapies, including Sitagliptin, and an increased incidence of pancreatic cancer (Butler et al., 2013).
Joint Pain: A Hidden Side Effect
Another risk that often flies under the radar is severe joint pain associated with Sitagliptin.
In 2015, the U.S. Food and Drug Administration (FDA) issued a warning that DPP-4 inhibitors, including Sitagliptin, could cause disabling joint pain.
This side effect can be so severe that patients might need to discontinue the medication.
While not everyone experiences this, it is a serious enough issue to warrant attention.
Heart Failure: The Unexpected Twist
Sitagliptin was initially thought to be safe for the heart, but more recent research has thrown a wrench into that assumption.
In 2016, a study published in The New England Journal of Medicine found that Sitagliptin was associated with an increased risk of hospitalization for heart failure in patients with type 2 diabetes (Scirica et al., 2013).
This finding was particularly concerning because cardiovascular safety is a major consideration in diabetes management.
Kidney Function: A Subtle but Serious Concern
Kidney function is another area where Sitagliptin may pose risks, especially for patients with pre-existing kidney issues.
While Sitagliptin is generally well-tolerated, there have been reports of worsening kidney function in some patients.
The drug is excreted by the kidneys, so if kidney function is compromised, Sitagliptin can accumulate in the body, potentially leading to toxicity.
The Debate: Experts Weigh In
Given these risks, it is no surprise that the medical community is divided on Sitagliptin’s safety profile.
Some experts argue that the benefits outweigh the risks, particularly for patients who don’t respond well to other treatments.
However, others are more cautious, suggesting that Sitagliptin should be used sparingly, especially in patients with a history of pancreatitis, heart failure, or kidney disease.
Dr. Steven Nissen, a prominent cardiologist, has voiced concerns about the cardiovascular risks associated with Sitagliptin, emphasizing the need for more robust clinical trials to fully understand its safety profile.
On the other hand, Dr. John Buse, a leading endocrinologist, points out that while the risks are real, they are relatively rare and must be weighed against the benefits on a case-by-case basis.
The Alternatives: Is There a Safer Option?
If the potential risks of Sitagliptin have you feeling uneasy, you are not alone.
The good news is that there are alternatives available, each with its own set of benefits and risks. Here are a few options to consider:
Metformin: The Tried and Tested
Metformin tablet is widely recognized as the go-to first-line treatment for type 2 diabetes, thanks to its strong track record of safety and effectiveness.
It primarily works by decreasing glucose production in the liver and enhancing the body’s sensitivity to insulin, making it easier to control blood sugar levels.
Unlike Sitagliptin, Metformin doesn’t carry risks like pancreatitis or heart failure.
However, it is not entirely without drawbacks.
Common side effects include gastrointestinal discomfort, and there is also the potential for a decrease in vitamin B12 levels, which requires monitoring.
SGLT2 Inhibitors: The New Kid on the Block
SGLT2 inhibitors, such as Empagliflozin and Canagliflozin, have quickly risen to prominence in the diabetes treatment world, thanks to their dual ability to lower blood sugar and offer heart-protective benefits.
These medications work by preventing the kidneys from reabsorbing glucose, allowing excess sugar to be excreted through urine. While this approach is innovative, it is not without its pitfalls.
Patients should be aware of the increased risks, including a higher likelihood of urinary tract infections and the potential for developing diabetic ketoacidosis, a serious condition that requires immediate medical attention.
Despite their benefits, these risks make it essential to use SGLT2 inhibitors with caution.
GLP-1 Receptor Agonists: The Heavy Hitters
GLP-1 receptor agonists, including Liraglutide (Victoza) and Semaglutide (Ozempic), have emerged as powerful alternatives in diabetes management.
These medications work by enhancing insulin secretion while simultaneously suppressing glucagon release, effectively helping to regulate blood sugar levels.
Beyond their glucose-lowering capabilities, GLP-1 agonists have also been linked to a reduced risk of cardiovascular events, offering a significant advantage for heart health.
However, they are not without side effects—common issues include nausea, and in rare instances, these drugs can lead to pancreatitis, a serious condition that requires immediate medical intervention.
Despite these risks, their benefits make them a compelling option for many patients.
FAQs on Sitagliptin for Diabetes Management
Q-1: Could sitagliptin’s effect on the immune system present unexpected risks for diabetic patients?
A-1: Emerging insights suggest sitagliptin may subtly influence immune function by modulating incretin hormones, which interact with immune cells. While rare, this modulation could theoretically increase susceptibility to certain infections or inflammatory reactions in sensitive individuals. However, these effects are not well-documented clinically and warrant careful monitoring rather than immediate concern.
Q-2: Is there a potential link between sitagliptin and cardiovascular risks that is underrecognized?
A-2: Although sitagliptin is generally considered safe for the heart, some studies have raised questions about a slight increase in heart failure risk in certain patients, especially those with pre-existing cardiac conditions. This hidden risk may not be immediately apparent and underscores the importance of cardiovascular evaluation before and during treatment.
Q-3: Can sitagliptin interfere with pancreatic health beyond common side effects?
A-3: There is ongoing investigation into whether sitagliptin could contribute to subtle pancreatic changes, such as inflammation or altered enzyme levels, which might not present obvious symptoms initially. While severe pancreatic issues are rare, this possibility highlights the need for vigilance in patients reporting abdominal discomfort or digestive changes.
Q-4: Does sitagliptin impact renal function in ways that might be overlooked in routine diabetes care?
A-4: Sitagliptin is excreted primarily through the kidneys, and in patients with compromised renal function, it may accumulate, increasing the risk of side effects. As per bestdietarysupplementfordiabetics.com research, “This hidden risk emphasizes the necessity for dose adjustments and regular kidney function monitoring to prevent potential toxicity or worsening renal impairment”.
Q-5: Are there concerns about sitagliptin contributing to subtle metabolic imbalances beyond glucose control?
A-5: Beyond lowering blood sugar, sitagliptin may influence other metabolic pathways, including lipid profiles and weight regulation, in ways not fully understood. Some patients might experience unexpected shifts in cholesterol levels or minor weight changes, which could impact overall metabolic health and diabetes management if not closely observed.
Conclusion: Is Sitagliptin the Hidden Risk?
So, is Sitagliptin truly the hidden risk in diabetes treatment?
The answer is not as straightforward as we would like.
Sitagliptin does offer notable benefits in managing blood sugar levels, making it a popular choice for many.
However, it is impossible to overlook the potential risks associated with its use. Issues like pancreatitis, pancreatic cancer, severe joint pain, heart failure, and kidney complications are serious concerns that require thoughtful consideration.
The important thing here is not to hit the panic button, but to stay informed.
If you are currently taking Sitagliptin or considering it, the best course of action is to have a candid conversation with your healthcare provider.
They can help you assess the pros and cons based on your unique health profile and guide you toward the best decision for your situation.
Managing diabetes is ultimately about finding the right balance—one that works for you.
For some, Sitagliptin might be a safe and effective option, especially when combined with a natural Blood Sugar Support Supplement, as I do in my own routine.
Please Note: I also include the Best Supplements to Lower Blood Sugar to keep my Type 2 diabetes in check.
For others, it might be wiser to explore alternative treatments. Whatever path you choose, ensure it is a well-informed decision that puts your long-term health and well-being first.
References: