DASH Diet Basics for Diabetes
- admin
- November 8, 2025
- 12:33 pm
- No Comments

The DASH diet (Dietary Approaches to Stop Hypertension) is not a fad or a gimmick.
It was built in clinics to reduce high blood pressure and then embraced widely because it improves overall diet quality, weight control, and heart-health markers.
For diabetes, that is a win on multiple fronts: blood pressure and cardiovascular risk are tightly linked to long-term outcomes, and many people with diabetes also aim to improve lipids and waist circumference.
DASH is simple: think vegetables and fruit at most meals, legumes and whole grains for fiber, fish and lean proteins for satiety, and low-fat dairy for calcium and protein—prepared with mostly unsaturated fats.
It deliberately trims sodium and added sugar while keeping saturated fat modest.
The pattern is flexible, familiar, and easy to personalize to your culture, budget, and kitchen skills.
You don’t need to micromanage every gram; you organize meals around food groups and portions that are practical to repeat.
Current clinical guidance treats DASH alongside Mediterranean-style eating as a first-line, evidence-based option that can be tailored to glucose targets and medications.
This guide by bestdietarysupplementfordiabetics.com distills exactly what DASH is, why it helps in diabetes, and how to start today—without filler.
Points Covered in this Article
- What DASH Is (and isn’t)
- Why DASH Helps in Diabetes
- Evidence in Plain Language
- Core Food Groups and Daily Servings
- The Mineral Engine: Sodium, Potassium, Magnesium, Calcium
- Building Plates and a Sample Day
- Shopping List and Smart Swaps
- Safety, Medications, and Special Cases
- A Four-Week Starter Plan
- Troubleshooting Highs, Lows, and Plateaus
- Tracking Progress: A1C, BP, Lipids, Weight
- Long-Term Maintenance
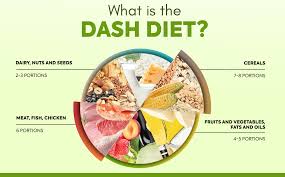
What DASH Is (and isn’t)?
DASH is a pattern, not a short detox. It emphasizes:
- Vegetables and fruit most days and most meals.
- Legumes, whole grains, nuts, and seeds for fiber, micronutrients, and steady energy.
- Low-fat or fat-free dairy for calcium and protein.
- Fish, poultry, and lean meats in measured portions.
- Unsaturated fats (olive/canola oils) in place of butter or ghee.
- Lower sodium and minimal added sugars.
A standard ~2,000-kcal DASH day typically targets: 6–8 servings grains (mostly whole), 4–5 vegetables, 4–5 fruit, 2–3 low-fat dairy, up to ~6 oz total lean meats/fish/eggs, 2–3 servings fats/oils, nuts/seeds/legumes several times weekly, and sweets sparingly.
What DASH isn’t: It’s not inherently low-carb or low-fat. It’s fiber-dense, plant-forward, and sodium-sensible. For diabetes, you can easily tune carbohydrate portions by shifting the mix toward legumes and non-starchy vegetables and away from refined grains.
Why DASH Helps in Diabetes?
Blood pressure control:
Hypertension is common in diabetes and magnifies cardiovascular risk. DASH reliably lowers systolic and diastolic blood pressure—often within weeks—because it prioritizes potassium-rich produce, low-fat dairy, and modest sodium.
Better glycemia and insulin sensitivity:
A plate built on vegetables, legumes, fruit, and intact grains slows carbohydrate absorption, flattens post-meal spikes, and supports improved insulin action. Many people see steadier energy, fewer cravings, and more predictable meter or CGM traces.
Lipids and weight:
Replacing refined starches and saturated fat with high-fiber plant foods and mostly unsaturated fat can lower triglycerides, nudge HDL upward, and support gradual weight loss or maintenance—especially when combined with basic activity.
Adherence:
The biggest lever is what you can sustain. DASH uses ordinary foods, flexible recipes, and household measures. That practicality translates to better long-term A1C and blood-pressure control.
Evidence in Plain Language
- Controlled feeding studies demonstrated that a pattern rich in vegetables, fruit, and low-fat dairy and lower in saturated fat reduces blood pressure even without weight loss.
- Reducing sodium on top of the DASH pattern lowers blood pressure further, with the largest benefits at lower sodium intakes for those who are salt-sensitive.
- In people with type 2 diabetes, clinical trials and reviews report improvements in insulin sensitivity, A1C, triglycerides, and blood pressure when participants adopt a DASH-aligned eating pattern.
- Major professional guidelines endorse DASH or Mediterranean-style patterns as evidence-based options for glycemic and cardiometabolic goals, with personalization to medications and preferences.
You do not need to memorize journals to benefit from this: follow the core food pattern and sodium guidance and measure your results.
Core Food Groups and Daily Servings
Use these as anchors, then scale to your energy needs and glucose goals:
- Grains (6–8/day): Prefer whole grains—oats, barley, brown rice, bulgur, whole-grain bread. One serving is typically 1 slice bread or ½ cup cooked grain.
- Vegetables (4–5/day): Load up on leafy greens, crucifers (broccoli, cauliflower), peppers, tomatoes, carrots, and mixed salads.
- Fruit (4–5/day): Whole fruit over juice for fiber and satiety. Pair with yogurt or nuts to blunt glycemic rise.
- Low-fat dairy (2–3/day): Milk, yogurt, or kefir. Choose plain, then flavor with cinnamon, fruit, or a drizzle of honey when needed.
- Lean proteins (≤6 oz/day): Fish, poultry, eggs; include fish several times per week.
- Nuts/seeds/legumes (ideally most days): Beans, lentils, chickpeas, almonds, walnuts, pumpkin seeds.
- Fats/oils (2–3/day): Use olive or canola oil generously enough for flavor but measured for calories.
- Sweets (sparingly): Define portions, prefer fruit-forward or lower-sugar options, and avoid sugary drinks.
Diabetes-friendly tweak: replace a portion of grains with legumes and add extra non-starchy vegetables; pair carbs with protein and healthy fat; and plan a short post-meal walk to smooth spikes.
The Mineral Engine: Sodium, Potassium, Magnesium, Calcium
- Sodium: Set a ceiling of ≤2,300 mg/day. Many with hypertension benefit from ~1,500 mg/day, but choose a target that is realistic and safe for you. Restaurant meals, breads, sauces, cured meats, and packaged snacks are the biggest stealth sources.
- Potassium: Abundant in vegetables and fruit (bananas, oranges, tomatoes, potatoes, leafy greens). Potassium helps balance sodium’s effects on blood pressure.
- Magnesium: Found in legumes, nuts, seeds, and whole grains; supports vascular tone and glucose metabolism.
- Calcium: Supplied mainly by low-fat dairy or fortified alternatives; contributes to blood-pressure benefits and bone health.
The DASH pattern works partly because it rebalances minerals while improving overall diet quality.
Building Plates and a Sample Day
The plate method (DASH-style, diabetes-aware)
- ½ plate: non-starchy vegetables (raw or cooked).
- ¼ plate: protein (fish, poultry, tofu/tempeh, eggs; legumes can serve as protein).
- ¼ plate: whole grains or extra legumes/starchy veg in measured portions.
- Add a fruit serving and/or a low-fat dairy serving where it fits your targets.
Sample one-day menu (~2,000 kcal; scale portions to your needs)
Breakfast:
- Plain low-fat yogurt with mixed berries and chopped walnuts
- ½ cup cooked oats stirred with cinnamon
- Coffee or tea, unsweetened
Snack:
- Apple plus a small handful of almonds
Lunch:
- Big Greek-style salad: leafy greens, cucumbers, tomatoes, peppers, olives, red onion, grilled salmon or tofu, olive-oil–lemon vinaigrette
- Small whole-grain pita
Snack:
- Carrot sticks with hummus or an orange
Dinner:
- Lentil-vegetable stew (onion, celery, carrots, tomatoes, spinach)
- Tray-roasted broccoli and carrots with olive oil and pepper
- ½ cup cooked barley or farro
- Glass of low-fat milk or plain lassi
Occasional dessert:
- Berries with a spoonful of plain yogurt or a square of dark chocolate
Label tips: prioritize low added sugar, high fiber, and shorter ingredient lists. For starches, watch portion size and pair with protein or fat. A 10–20-minute after-dinner walk is a simple glycemic lever.
Shopping List and Smart Swaps
Produce:
- Leafy greens; broccoli/cauliflower; tomatoes; cucumbers; peppers; onions; citrus; apples; bananas; berries; herbs (cilantro, parsley, basil).
Pantry:
- Dried/canned beans and lentils (no-salt-added when possible), oats, brown rice, barley, bulgur, whole-grain bread or rotis with short ingredient lists.
Proteins:
- Salmon, sardines, white fish; skinless chicken or turkey; eggs; tofu/tempeh; plain low-fat yogurt and milk.
Fats and flavor:
- Olive/canola oils; nuts and seeds; vinegars; mustard; tahini; garlic; ginger; lemon/lime; salt-free spice blends.
High-impact swaps:
- Butter → olive oil
- Refined breads → whole-grain options
- Salty snacks → unsalted nuts or roasted chickpeas
- Processed meats → fish or skinless poultry
- Sugary drinks → water, sparkling water, or unsweetened tea/coffee
Safety, Medications, and Special Cases
Insulin or sulfonylureas:
As you improve carbohydrate quality and overall pattern, mealtime insulin requirements often fall. Plan for closer monitoring during the first weeks and coordinate dose adjustments to prevent hypoglycemia.
Blood-pressure medications:
DASH and sodium reduction can improve readings fairly quickly. Track BP at home and discuss any consistent drops to avoid overtreatment.
Chronic kidney disease:
Lactose intolerance:
Opt for lactose-free milk or yogurt, or consider fortified alternatives to maintain calcium intake while preserving the DASH structure.
Cultural fit:
DASH is a template, not a cuisine. Indian, Middle Eastern, and Latin plates map well: think dal and chana; vegetable-forward thalis; grilled fish with beans and salads; olive-oil-based mezze; rice and grain portions tuned to your glucose goals.
A Four-Week Starter Plan
Week 1 — Stock & Simplify:
- Stock beans/lentils, intact grains, low-sodium canned tomatoes/beans, frozen vegetables, plain yogurt, and two oils (olive for most uses, canola for neutral cooking).
- Move to ½-plate vegetables at lunch and dinner.
- Replace butter and heavy sauces with olive oil, herbs, citrus, and vinegar.
- Begin a sodium scan: compare labels, choose “no-salt-added” when possible, and track an estimate of daily sodium.
Week 2 — Protein Rhythm & Fiber:
- Plan fish 2–3 times this week.
- Add two legume meals (dal, lentil soup, chickpea salad, bean-and-veg bowls).
- Target 25–30 g fiber/day with vegetables, fruit, legumes, oats/barley, and nuts/seeds.
- Add 10–20-minute post-meal walks once or twice daily.
Week 3 — Sodium Trim & Sugar Audit:
- Swap high-sodium snacks and processed meats for fresh options. Rinse canned beans to reduce sodium further.
- Audit added sugars in breakfast items, sauces, and beverages; choose plain dairy and add fruit yourself.
- If BP drops noticeably, discuss medication adjustments.
Week 4 — Personalize & Plan Ahead:
- Lock in 6–8 go-to meals you enjoy and can cook quickly.
- Fine-tune grain portions using CGM or meter patterns; substitute legumes or extra non-starchy vegetables where spikes persist.
- Set a standing grocery list and a weekly prep block (batch-cook beans/grains, roast vegetables, portion nuts).
Troubleshooting Highs, Lows, and Plateaus
Post-meal highs:
- Halve refined grains; bias toward legumes + non-starchy veg; add protein and a drizzle of olive oil; check drinks and sauces for hidden sugars.
- Try a 10–20-minute walk after the meal.
Frequent lows (if on insulin/SU):
- New meals may need less mealtime insulin. Carry fast carbs, set conservative alerts on your meter/CGM, and coordinate dose changes.
Weight plateau:
- Audit calorie-dense foods (oils, nuts, cheese). Keep olive oil but measure; keep nuts but pre-portion.
- Add resistance training 2–3 times weekly and push daily steps.
BP not budging:
- Re-check sodium sources (restaurant meals, bread, cured meats, condiments). Move closer to ~1,500 mg/day if appropriate and add more potassium-rich produce.
Cravings:
- Increase protein at meals and lead with a veg-or-bean starter (salad or soup) to improve fullness.
Tracking Progress: A1C, BP, Lipids, Weight
- Blood pressure: Expect meaningful changes in 2–4 weeks, faster with sodium reduction. Track at home at the same times daily.
- Glucose/A1C: Look for smaller post-meal rises within 2–6 weeks. Early A1C shifts appear by about 12 weeks of consistency.
- Lipids: Triglycerides often fall and HDL may improve with plant-forward, lower-saturated-fat patterns.
- Weight & waist: If weight loss is a goal, trim liquid calories, tighten portions of calorie-dense foods, and increase daily movement.
- How you feel: Energy between meals, fewer evening cravings, and better sleep are practical signals that the pattern fits.
Long-Term Maintenance
- Keep the template; rotate flavors. Use the same structure across cuisines—vegetable-heavy plates, legumes frequently, whole grains in measured portions, low-fat dairy, fish and lean proteins, low sodium, minimal added sugar.
- Batch, freeze, and portion. Cook beans and grains in bulk; roast vegetables on trays; portion nuts and hummus.
- Restaurant playbook: Lead with protein + veg, request double veg instead of fries, ask for sauces on the side, and choose grilled/baked over fried.
- Review quarterly. Revisit A1C, home BP readings, lipids, weight, and how you feel. Tweak sodium, portions, and activity to match your goals and medication plan.
Conclusive Analysis
The DASH diet gives people with diabetes a straightforward, sustainable way to improve blood pressure, glycemia, and heart risk—without exotic rules or expensive products.
Its power comes from everyday foods: vegetables and fruit, legumes and whole grains, low-fat dairy, lean proteins, and mostly unsaturated fats, with sodium and added sugars kept in check.
You can personalize carbohydrate portions easily by leaning on legumes and non-starchy vegetables and trimming refined starches.
Expect blood-pressure benefits within weeks and glycemic improvements as consistent patterns take hold.
If you use insulin or sulfonylureas, coordinate dose changes as meals improve to prevent lows.
Stock smart staples, master a handful of repeatable meals, and use your meter or CGM to guide fine-tuning.
Keep prep simple, break up sitting time with short walks, and track the markers that matter to you.
Done consistently, DASH becomes less of a “diet” and more of a durable, enjoyable way to eat for steadier glucose and stronger heart health.
References: