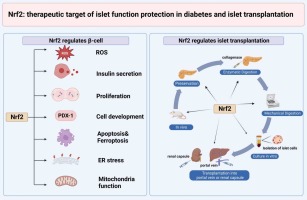
Pancreatic beta cells play a crucial role in regulating blood glucose levels through insulin secretion.
Maturity-Onset Diabetes of the Young (MODY) is a monogenic form of diabetes, typically resulting from mutations in genes associated with beta-cell function.
This article explores the mechanisms by which these mutations lead to MODY diabetes, highlighting the genetic, molecular, and functional disruptions that occur.
We will discuss the specific genes involved, their impact on beta-cell operations, and real-life examples illustrating the clinical presentation and management of MODY.
Article Index:
- Introduction to MODY and Beta-Cell Function
- Key Genes Implicated in MODY
- Mechanisms of Beta-Cell Dysfunction in MODY
- Impaired Glucose Sensing in MODY Beta Cells
- Real-Life Example: Sarah’s MODY Diagnosis
- Long-Term Implications of Beta-Cell Mutations in MODY
- Diagnostic Tools for Identifying MODY-Linked Beta-Cell Mutations
- FAQs on Pancreatic Beta-Cell Mutations & MODY Diabetes
- Research Supporting Beta-Cell Dysfunction in MODY
Introduction to MODY and Beta-Cell Function
MODY is a rare form of diabetes caused by mutations in at least 14 identified genes, most of which are expressed in pancreatic beta cells.
These mutations disrupt the delicate processes of glucose sensing, insulin gene expression, and secretion.
Unlike Type 1 or Type 2 diabetes, MODY is inherited in an autosomal dominant manner, typically presenting before the age of 25.
Beta cells in the pancreas are specialized for insulin production and release in response to blood glucose levels.
This dynamic balance is disrupted when mutations occur in MODY-associated genes, resulting in persistent hyperglycemia and impaired metabolic control.
Key Genes Implicated in MODY
MODY is primarily associated with mutations in three key genes:
- HNF1A (MODY3): This gene encodes a transcription factor critical for beta-cell development and insulin secretion. Mutations reduce beta-cell efficiency, leading to glucose intolerance.
- GCK (MODY2): Glucokinase, a glucose sensor in beta cells, is encoded by this gene. Mutations impair the conversion of glucose to glucose-6-phosphate, disrupting normal insulin release.
- HNF4A (MODY1): This gene regulates insulin production and beta-cell differentiation, with mutations leading to progressive diabetes.
Other genes such as HNF1B, INS, and KCNJ11 also contribute to MODY, albeit less frequently.
Mechanisms of Beta-Cell Dysfunction in MODY
Here is how it all takes shape:
Impaired Insulin Gene Expression:
Beta-cell mutations in genes like HNF1A and HNF4A interfere with transcriptional regulation critical for insulin production.
These mutations reduce the production of insulin mRNA, impairing insulin synthesis despite elevated glucose levels.
This results in insufficient insulin secretion, a hallmark of MODY.
Defective Glucose Sensing:
Mutations in the GCK gene, which encodes glucokinase, compromise the beta cell’s ability to sense blood glucose levels accurately.
Glucokinase acts as a glucose “sensor,” triggering insulin release.
Dysfunction in this enzyme shifts the glucose threshold for insulin secretion, leading to stable but elevated fasting glucose levels, characteristic of MODY2.
Beta-Cell Exhaustion:
Persistent attempts by beta cells to maintain glucose homeostasis result in overwork and eventual failure.
This phenomenon is particularly evident in MODY3, where insulin production declines progressively over time.
A study published in Diabetes Care emphasized that prolonged beta-cell dysfunction accelerates the decline in insulin secretion, often necessitating pharmacological intervention.
These mechanisms highlight the intricate genetic disruptions underlying MODY, reinforcing the need for precise diagnosis and tailored management to address beta-cell dysfunction effectively.
Impaired Glucose Sensing in MODY Beta Cells
The pancreas depends on accurate glucose sensing to regulate insulin secretion effectively. Glucokinase, an enzyme encoded by the GCK gene, plays a central role as the “glucose sensor” in pancreatic beta cells.
This enzyme determines the threshold at which glucose triggers insulin release, ensuring tight blood sugar control.
Mutations in the GCK gene reduce the enzyme’s activity, resulting in a higher glucose threshold for insulin secretion.
This means beta cells respond to glucose less effectively, leading to persistent but mild fasting hyperglycemia.
Unlike other forms of diabetes, MODY2 does not typically result in severe glucose fluctuations or complications.
A study in Diabetes (2019) highlighted that individuals with GCK mutations often present with stable blood sugar levels and are less likely to require pharmacological interventions.
This stability is a hallmark of MODY2, emphasizing the importance of understanding glucokinase’s function in diagnosing and managing the condition.
Real-Life Example: Emma’s MODY Diagnosis
Emma, a 20-year-old college student, began noticing frequent episodes of mild hyperglycemia during routine health check-ups.
Despite her family history of diabetes, her condition was initially misdiagnosed as Type 1 diabetes, leading to unnecessary insulin therapy.
Unsatisfied with her progress and seeking clarity, Emma consulted a specialist.
Her endocrinologist suspected MODY due to her family history and age of onset. Genetic testing revealed a GCK gene mutation, confirming a diagnosis of MODY2.
This mutation disrupted her beta cells’ glucose-sensing ability, leading to stable but elevated fasting glucose levels.
With this diagnosis, her treatment plan shifted. Instead of insulin, Emma managed her condition through lifestyle modifications, including a balanced diet and regular exercise.
Within months, she achieved stable blood glucose levels and felt more in control of her health.
Emma’s experience highlights the importance of genetic testing in identifying MODY and tailoring treatment accordingly.
Her case underscores how beta-cell mutations often present subtly, requiring precise diagnostic tools to avoid misdiagnosis and unnecessary treatments.
Accurate identification of MODY not only improved Emma’s quality of life but also guided preventive measures for her family members at risk.
Long-Term Implications of Beta-Cell Mutations in MODY
MODY diabetes presents unique challenges due to its genetic basis and progression, with implications for individual health and familial impact:
Progressive Beta-Cell Failure:
In MODY3, caused by mutations in the HNF1A gene, beta-cell functionality gradually deteriorates, leading to reduced insulin secretion.
As a result, patients often require pharmacological interventions like sulfonylureas, which help stimulate insulin release.
A study published in Diabetes Care emphasized the efficacy of these medications in maintaining glycemic control in MODY3 patients.
Risk of Secondary Complications:
Persistent hyperglycemia due to impaired insulin secretion elevates the risk of microvascular complications, including retinopathy (damage to the retina) and nephropathy (kidney dysfunction).
These risks are especially prominent in MODY1 and MODY3 patients, making early diagnosis and tight glycemic control crucial.
Research in Diabetologia highlights that untreated MODY patients are at a higher risk for these complications compared to those with Type 2 diabetes.
Generational Impact:
MODY’s autosomal dominant inheritance pattern means there is a 50% chance that an affected parent will pass the condition to their offspring.
Without proper diagnosis, family members may unknowingly live with MODY, increasing their risk of complications.
Early genetic screening for family members can identify at-risk individuals, enabling timely interventions to mitigate disease progression and improve outcomes.
Diagnostic Tools for Identifying MODY-Linked Beta-Cell Mutations
Diagnosing MODY diabetes involves a combination of genetic, familial, and biochemical evaluations to distinguish it from other types of diabetes:
- Genetic Testing: Advanced techniques like Next-Generation Sequencing (NGS) and Polymerase Chain Reaction (PCR) are pivotal in detecting mutations in MODY-associated genes such as HNF1A, GCK, and HNF4A. These tools provide a precise diagnosis by identifying the specific genetic cause.
- Family History Assessment: Since MODY follows an autosomal dominant inheritance pattern, understanding family history is critical. A pattern of diabetes onset in multiple generations before age 25 often indicates MODY.
- Biochemical Markers: Patients with MODY typically show persistent fasting hyperglycemia but lack markers of insulin resistance or autoimmune destruction, which differentiates it from Type 1 or Type 2 diabetes.
A study published in Endocrine Reviews highlights the value of genetic testing in achieving diagnostic accuracy.
This precision enables personalized treatment plans, ensuring patients receive appropriate therapies and preventing misdiagnosis, which could lead to unnecessary insulin use.
Combining these diagnostic tools enhances early detection and intervention, improving outcomes for MODY patients.
Research Supporting Beta-Cell Dysfunction in MODY
Numerous studies have delved into the relationship between beta-cell mutations and MODY, uncovering critical insights into the disease’s molecular underpinnings:
- Diabetologia (2020): This study demonstrated that mutations in the HNF1A gene significantly reduce transcriptional activity, impairing insulin production and secretion. The findings highlighted how such mutations disrupt beta-cell function, leading to glucose intolerance typical of MODY3.
- Journal of Clinical Endocrinology & Metabolism (2019): Research emphasized the role of GCK mutations in MODY2, showing how they alter the glucose threshold for insulin release. By affecting glucokinase activity, these mutations result in persistent but mild hyperglycemia, which is a hallmark of this MODY subtype.
- Nature Genetics (2018): This study revealed epigenetic changes in beta cells caused by MODY-associated mutations. These changes disrupt the expression of genes critical for insulin secretion, providing new insights into the progressive nature of MODY.
These studies collectively highlight the complexity of MODY, linking genetic mutations directly to impaired beta-cell function.
They also emphasize the need for targeted genetic research to improve diagnostic precision and therapeutic strategies, ensuring personalized care for individuals with MODY.
Understanding these mechanisms at the molecular level is essential for advancing treatments and improving patient outcomes.
FAQs on Pancreatic Beta-Cell Mutations & MODY Diabetes
Q-1: How do INS (insulin gene) mutations cause diabetes without classic autoimmunity?
A-1: Many INS variants make proinsulin fold incorrectly. Those misfolded proteins clog the endoplasmic reticulum, trigger a stress response, and interfere with secretion from even the normal gene copy—a “dominant-negative” effect. Over time the stressed β-cells falter, insulin output drops, and blood glucose rises, often with a high proinsulin-to-insulin or proinsulin-to-C-peptide ratio.
Q-2: Why do transcription-factor mutations (HNF1A, HNF4A, PDX1) look so different from GCK-MODY?
A-2: HNF1A/HNF4A/PDX1 control β-cell identity and the machinery for insulin gene expression. Mutations here blunt glucose-stimulated insulin secretion and make hyperglycemia progressively worse—yet often very responsive to low-dose secretagogues. GCK-MODY is different: one faulty glucokinase shifts the glucose “set-point,” causing mild, stable fasting hyperglycemia that rarely needs medication outside pregnancy.
Q-3: How can KATP-channel genes (KCNJ11/ABCC8) produce a MODY-like picture?
A-3: KCNJ11 and ABCC8 encode the β-cell KATP channel. Variants that keep the channel too open prevent proper depolarization and calcium entry, so insulin release lags despite normal glucose sensing. Although famous for neonatal diabetes, some variants present later with a MODY phenotype and can respond well to sulfonylureas.
Q-4: What quick lab or clinical clues point to a β-cell mutation rather than type 1 or type 2 diabetes?
A-4: Antibody-negative hyperglycemia at a young age plus an autosomal-dominant family pattern is the biggest breadcrumb. Additional hints: in GCK-MODY, mild fasting elevations from childhood with little progression; in INS-related disease, disproportionate hyperproinsulinemia; in HNF1A/HNF4A, striking sensitivity to low-dose sulfonylureas and pronounced post-meal spikes.
Q-5: Do genotype–therapy links really matter in day-to-day care?
A-5: Absolutely. HNF1A/HNF4A forms often respond dramatically to small doses of sulfonylureas or short-acting secretagogues; GLP-1–based therapy is useful when hypoglycemia risk or weight is a concern. GCK-MODY typically needs no medication. INS-MODY is variable; strategies that minimize β-cell stress (steady targets, protein- and fiber-forward meals, limiting large glucose swings) and earlier insulin in some cases help preserve control.
Q-6: Why is PDX1 frequently singled out in MODY discussions?
A-6: PDX1 is a master switch for pancreas development and adult β-cell identity. With one affected copy, it can cause MODY4 due to secretion defects of varying severity; with both copies lost, it can produce neonatal diabetes with profound pancreatic underdevelopment—illustrating how transcriptional control sits upstream of insulin production itself.
Takeaway: MODY arises when single-gene defects derail β-cell protein folding (INS), glucose sensing (GCK), stimulus-secretion coupling (KATP), or transcriptional identity (HNF1A/HNF4A/PDX1). Recognizing the pattern steers therapy—from “usually no drugs” (GCK) to secretagogue-responsive (HNF1A/HNF4A/KATP) to stress-minimizing or early insulin strategies (INS)—and guides family screening.
Conclusion
Pancreatic beta-cell mutations are central to the development of MODY diabetes, disrupting glucose sensing, insulin gene expression, and secretion.
Accurate diagnosis through genetic testing and a thorough understanding of beta-cell dysfunction is crucial for effective management.
Emma’s case exemplifies the transformative impact of early detection and tailored treatment plans.
By focusing on the underlying genetic causes, healthcare professionals can provide targeted interventions, improving patient outcomes and quality of life.
References: