How to Take Extended Release Metformin Correctly?
- admin
- June 11, 2025
- 7:18 pm
- No Comments
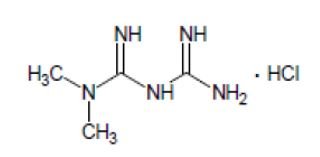
Extended‑release (ER) Metformin is a mainstay in the treatment of type 2 diabetes, offering a smoother blood concentration profile and improved gastrointestinal tolerability over the immediate‑release version.
However, for this medication to be both safe and effective, it is vital to take it exactly as directed.
Whether you are new to Metformin ER or looking to refine your routine, understanding the proper strategies—from timing and dosing to handling side effects—can make a big difference in your health outcomes and daily experience.
Index:
- Understanding the importance of correct dosing
- Best time to take ER Metformin
- How to start and increase your dosage
- Proper tablet use
- Handling missed doses
- Checking and protecting kidney function
- Managing temporary interruptions
- Tips for reducing side effects
- Transitioning between formulations
- Day‑to‑day strategies for consistency
- Common FAQs
- Final summary
Understanding the Importance of Correct Dosing
Taking ER Metformin correctly helps ensure that your blood sugar stays stable and minimizes unpleasant side effects like nausea or diarrhea.
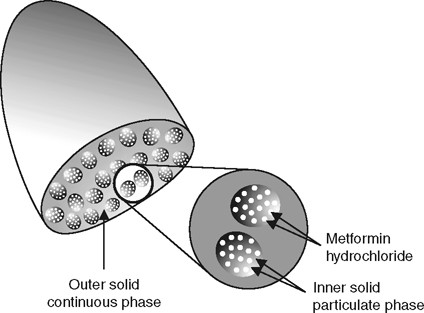
The extended‑release mechanism allows the medication to be absorbed slowly, avoiding sudden peaks that can disrupt your digestion.
Getting the dose and timing wrong—such as taking it on an empty stomach or altering the prescribed dose—can increase side effects or reduce effectiveness.
Conversely, following the guidelines accurately supports long‑term health benefits and better adherence to your diabetes management plan.
Best Time to Take Extended Release Metformin
The consensus across medical resources is that ER Metformin is most effective and best tolerated when taken once daily with your evening meal.
This timing takes advantage of two key factors:
- Digestive buffering: The presence of food slows down the absorption, reducing the likelihood of stomach upset or diarrhea.
- Stable blood sugar coverage: Taking it in the evening helps maintain blood glucose levels overnight and into the next day.
To build consistency, match it to your regular dinner time. If dinner varies (e.g., between 6 p.m. and 7:30 p.m.), pick a consistent hour and stick with it. If your weight or activity level changes, talk with your doctor before changing the timing.
How to Start and Increase Your Dosage?
Here is how you need to set the pace to ensure that your blood sugar levels remain under your control:
A. Start Low:
Most doctors recommend beginning with 500 mg once daily with dinner to see how your body adapts. Starting low gives your system time to adjust without overwhelming your digestive tract.
Some formulations or specific patient scenarios may call for beginning at 1,000 mg, but 500 mg is the most common and typically the most tolerable starting point.
B) Gradual Increase:
You shall most likely need more than 500 mg for blood glucose control, so a slow, methodical increase is key.
A typical approach is:
- Increase by 500 mg every 1–2 weeks, checking how you feel and monitoring fasting glucose levels each morning.
- Stop increasing once you reach a stable, effective dose—usually between 1,000–2,000 mg per day, taken all at once in the evening.
- Some people require up to 2,000 mg for ideal control. In rare cases where even more is needed, immediate‑release (IR) versions may allow slightly higher total daily doses.
C) Monitoring Progress:
As you increase the dose, track your blood sugar regularly and note any side effects, especially digestive issues.
If your readings are optimal and side effects minimal, maintain that dosage. If side effects interfere, pause dosage increases until symptoms subside.
Proper Tablet Use
ER Metformin tablets are designed to be swallowed whole.
Here is how to take them properly:
- Do not crush, split, or chew the tablet—this would release the entire dose at once, defeating the extended‑release purpose and increasing risk of side effects.
- Take it with a full glass of water during your evening meal. Adequate hydration helps ensure the tablet dissolves slowly as intended.
- If swallowing pills is difficult, talk with your doctor about alternatives like mixing with soft food or switching to a different formulation—never crush or chew.
Handling Missed Doses
It is common to occasionally forget a medication—that is okay.
Here is how to manage missed doses:
- If you remember early in the evening, after dinner and well before bedtime, take the dose right away.
- If it’s getting late or close to your next dose, skip the missed pill and resume your regular schedule the following evening.
- Never double the dose to make up for a missed pill. Taking two can increase side effects and disrupt your blood sugar balance.
- Keeping a medication tracker—either a physical checklist or an app—can help prevent missed doses.
Checking and Protecting Kidney Function
Proper kidney function is essential when using Metformin, including ER forms.
There are certain risks involved in taking extended release metformin that you need to take into account.
Why Monitor eGFR?
Metformin is cleared through the kidneys. If kidney function is reduced, the drug can accumulate and increase the risk of lactic acidosis—a rare but dangerous complication. As a result:
- Before starting ER Metformin, it’s standard to measure your estimated glomerular filtration rate (eGFR):
- If eGFR is below 45 mL/min/1.73 m², your doctor may adjust the dose or choose a different treatment.
- If eGFR is below 30, ER Metformin is generally contraindicated.
How Often Should You Check?
- Yearly checks are typical for most patients.
- For elderly individuals or those with other health risks, more frequent monitoring may be recommended.
Before Procedures or Illness:
If you are scheduled for a procedure involving contrast dye, or if you are experiencing serious illness—like severe dehydration, infection, or cholesterol induced low blood pressure—your doctor may instruct you to temporarily pause Metformin ER.
Once you are stable and kidney function is rechecked within 48 hours, you can usually restart.
Managing Temporary Interruptions
Certain events call for a pause in taking Metformin ER, such as:
- Acute illness (severe vomiting, fever, dehydration)
- Hospitalization or surgeries requiring fasting
- Severe congestive heart failure or respiratory problems
During these times, kidney clearance may decrease, making it safer to hold the medication.
When you are recovering, drinking fluids with food, ensuring stable kidney readings, and then restarting as instructed ensures safe resumption with minimal risk.
Tips for Reducing Side Effects
Even while taking it correctly, Metformin ER can sometimes cause side effects.
Here are practical ways to reduce them:
- Start low and slow: Begin with 500 mg and increase gradually. This allows your body to adapt.
- Take with dinner every day: The food buffers the medication during digestion.
- Stay well hydrated: Drink plenty of water to support kidney function and minimize digestive discomfort.
- Avoid crushing tablets: This prevents releasing the full dose at once.
- Switch to ER from IR: If you were on immediate‑release and experienced side effects, switching to extended‑release often eases those symptoms.
- Control diarrhea and nausea: These are often temporary and ease as your body adjusts.
- Avoid heavy alcohol: Drinking large amounts can interfere with glucose control and increase the risk of rare metabolic complications.
- Check vitamin B12 levels occasionally: Long‑term use of Metformin has been linked to lower B12 levels, so monitoring and supplementation may be beneficial.
Transitioning Between Formulations
If you are considering switching between immediate‑release and extended‑release formulations:
From Instant Release to Extended Release:
- Keep the same total daily dose, up to 2,000 mg in one ER dose.
- Monitor your blood sugar and side effects during the first 4–6 weeks. Dosage can be adjusted based on results.
- If larger doses are still necessary for control, you can split the ER dose or revert to IR, which allows doses above 2,000 mg.
From ER to IR:
- Consider this if you cannot tolerate even the extended‑release tablets due to digestive sensitivity.
- Again, maintain total daily dosage initially, monitor blood sugar, and adjust as needed.
Changing formulations may improve tolerability or efficacy—but must be done under medical guidance.
Day‑to‑Day Strategies for Consistency
- Set reminders: Use alarms or apps to take your pill at the same time each day.
- Pair it with dinner: Habit‑stacking with a routine meal helps ensure you don’t forget.
- Track any patterns: Note when side effects occur and what’s on your plate—sometimes spicy or fatty foods can aggravate symptoms.
- Reassess when things change: Travel, new medications, stress, or changes in diet can affect how your body reacts.
- Keep open communication: Share any concerns or symptoms with your provider to adjust safely.
Common FAQs on Extended Release Metformin:
Q: Can I cut ER Metformin tablet in half?
A: No. Splitting or crushing the tablet destroys the extended‑release mechanism and may lead to uncomfortable side effects or reduced control.
Q: What if I forget to take it before dinner?
A: Take it as soon as you remember—unless it’s late. Never double up the next day; just continue your usual evening dose.
Q: Can I drink alcohol while on ER Metformin?
A: Moderate alcohol is usually okay, but excessive drinking increases risk of metabolic complications. Always discuss with your doctor, especially if you drink heavily.
Q: How will I know when to increase my dose?
A: Your healthcare provider will guide this based on blood sugar readings, A1C levels, and side effect tolerance.
In general, if your fasting glucose is still above target and side effects are manageable, your provider may recommend increasing by 500 mg.
Q: Is Metformin ER safe during pregnancy or breastfeeding?
A: Metformin is sometimes used in pregnancy for gestational diabetes, but decisions about formulation should be made with your doctor. ER is often an option, but individual circumstances vary.
Q: Can I stop taking it once my A1C is normal?
A: Even if your A1C is in range, stopping Metformin without consulting a doctor can lead to rebound high blood sugar. Usually, it’s continued long‑term unless another therapy is substituted or circumstances change.
Final Summary
Taking Metformin ER correctly is simple but important.
Here is a recap of the ideal approach:
- Start low (usually 500 mg with dinner) and increase by 500 mg every 1–2 weeks until blood sugar targets are met.
- Take it with your evening meal, every night, accompanied by a full glass of water.
- Swallow the tablet whole—do not crush, split, or chew.
- Stay consistent and hydrated, especially as kidney function is monitored.
- Skip missed doses without doubling up, and use reminders to stay on schedule.
- Pause the medication during acute illness, dehydration, or before invasive procedures, restarting once you’re stable.
- Monitor B12 levels and limit alcohol intake to avoid complications.
By following this routine—timing it right, dosing progressively, swallowing it properly, and watching your body’s signals—you shall maximize the benefits of ER Metformin while minimizing discomfort or risk.
Always work closely with your healthcare provider and regularly monitor your blood sugar and kidney function for the safest, most effective long‑term management of type 2 diabetes.
Concluding Thoughts
Extended‑release Metformin is a powerful and well‑tolerated medication when used correctly.
It is not just about taking a pill—it is about committing to a smart, consistent routine that supports your overall health.
With proper timing, gradual dosage adjustments, informed pill handling, and attentive monitoring, you empower yourself to stay in control of your diabetes with fewer side effects and better quality of life.
Keep this guide as a checklist alongside your healthcare provider’s instructions and do club metformin with a blood sugar support supplement to derive maximum benefits.
By staying informed and intentional about your medication routine—especially with ER formulations—you can truly reap the full benefits of
Metformin in your journey toward stable blood glucose management.
References: