How Type 2 Diabetes Disrupted My Glucose Metabolism?
- admin
- October 17, 2024
- 7:44 am
- No Comments

It was one of those routine doctor visits that ended up changing my life.
I had always heard about type 2 diabetes, but like most people, I thought it was something that happened to others.
I had no idea how closely my daily habits and choices were connected to my body’s internal systems—specifically, glucose metabolism.
When my doctor explained that I had type 2 diabetes, I did not immediately grasp the full implications. I knew it meant something about blood sugar, but what I didn’t understand was how deeply this condition would impact my life by disrupting my glucose metabolism.
Over the next few months, I would learn exactly how glucose metabolism in type 2 diabetes works—or more accurately, does not work.
And as I adjusted my lifestyle, I began to piece together the complex interaction between glucose, insulin, and the body’s metabolic pathways.
It was a difficult journey, but understanding how type 2 diabetes disrupted my glucose metabolism was the first step to taking control of my health.
Points Covered in this Article:
- Introduction to Glucose Metabolism
- How Glucose Metabolism Works: A Crash Course
- Type 2 Diabetes and Impaired Glucose Metabolism
- How Lifestyle Choices Impacted My Glucose Metabolism
- Scientific Explanation of the Metabolic Pathways Involved in Diabetes
- FAQs on Type 2 Diabetes & Glucose Metabolism
- Conclusion: Rebalancing Glucose Metabolism and Managing Type 2 Diabetes
Introduction to Glucose Metabolism
Glucose metabolism is central to how our bodies function. Every cell in our body needs energy to operate, and that energy comes from glucose, a type of sugar derived from the foods we eat.
The way our body processes glucose—by turning it into energy—relies heavily on a hormone called insulin. For people without diabetes, this process happens effortlessly. But for those of us with impaired glucose metabolism, like in my case, it is a completely different story.
When you have type 2 diabetes, your body’s ability to process glucose is disrupted. This disruption stems from insulin resistance or insufficient insulin production, leading to elevated blood sugar levels over time.
The more I learned about the mechanics of this, the more I realized just how much my body was struggling to manage glucose.
How Glucose Metabolism Works: A Crash Course
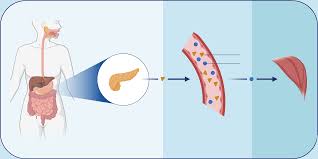
In a healthy body, after you eat a meal, your digestive system breaks down the carbohydrates into glucose. This glucose is released into the bloodstream, raising metabolic glucose levels.
The pancreas detects this spike and releases insulin to help shuttle the glucose into your cells, where it can be used for energy.
This process is what we call glucose insulin metabolism—a finely tuned dance between glucose and insulin that keeps your blood sugar stable.
In a nutshell, glucose metabolism and insulin work together like a lock and key. Insulin acts as the key that “unlocks” the door to your cells, allowing glucose to enter and fuel your body’s activities.
But when you have type 2 diabetes, this elegant system becomes faulty. Either the lock (your cells) becomes resistant to insulin, or the key (insulin) is in short supply.
As a result, glucose can’t get into the cells, and it builds up in the bloodstream, leading to chronically high blood sugar levels.
Type 2 Diabetes and Impaired Glucose Metabolism
Type 2 diabetes is not just about high blood sugar—it is about a breakdown in how the body processes glucose. At the center of this dysfunction is insulin, the hormone responsible for regulating blood sugar levels.
When the system goes off track, it leads to a cascade of metabolic problems that, over time, can affect nearly every major organ.
Let us break this down with scientific insight and real-world clarity:
Insulin Resistance: The Starting Point
In type 2 diabetes, the body becomes resistant to insulin. That means even though the pancreas still produces insulin, the body’s cells do not respond to it efficiently. It is like trying to open a locked door with a bent key—insulin is present, but it cannot do its job properly.
According to a 2021 study published in The Lancet Diabetes & Endocrinology, insulin resistance often develops years before a formal diagnosis of diabetes.
Example: Imagine a delivery truck (insulin) trying to drop packages (glucose) into houses (cells), but the gates are rusted shut. The packages pile up in the streets (bloodstream), causing traffic jams (hyperglycemia).
Pancreatic Overcompensation:
To deal with this inefficiency, the pancreas starts pumping out more insulin to overcome resistance. Initially, this compensatory mechanism keeps blood sugar in check. However, it puts tremendous strain on the pancreatic beta cells. Mutations to beta cells cause MODY, which is why you need to keep things in check.
Example: It is like turning up the volume on a broken speaker—it might work temporarily, but you’re only making the system wear out faster.
Beta Cell Burnout:
Over time, the pancreas simply cannot keep up. The beta cells become dysfunctional or die off. A 2020 review in Diabetologia confirmed that declining beta-cell function is a major driver in the transition from prediabetes to full-blown diabetes.
Glucose Stuck in the Bloodstream:
With both poor insulin sensitivity and reduced insulin production, glucose has nowhere to go—it lingers in the bloodstream. This chronic hyperglycemia is what causes long-term complications.
Example: Think of glucose like fuel—if it cannot get into the engine (cell), it does not power anything. Instead, it just sits there, corroding the tank.
Organ and Tissue Damage:
Persistently high glucose acts like a slow poison. It binds to proteins in the blood, forming advanced glycation end-products (AGEs), which damage blood vessels, nerves, kidneys, and the eyes.
This explains why people with poorly controlled diabetes are at higher risk for heart disease, neuropathy, and retinopathy.
Type 2 diabetes is not just a sugar issue—it is a systemic failure of insulin signaling and cellular glucose uptake.
By understanding this chain reaction, from insulin resistance to beta cell burnout, we can better appreciate why early intervention, lifestyle changes, and glucose monitoring are essential to prevent serious complications.
How Lifestyle Choices Impacted My Glucose Metabolism?
I never thought my day-to-day lifestyle choices were setting the stage for type 2 diabetes. I was not particularly overweight, and I exercised (jogging to control blood glucose levels) on occasion.
But when I examined my diet and habits more closely, it became clear how they were contributing to impaired glucose metabolism.
Take my diet, for example. I relied heavily on quick, convenient foods that were high in refined sugars and simple carbohydrates—things like white bread with avocado, sugary snacks, and processed meals.
These types of foods cause a rapid spike in blood sugar, forcing my body to produce large amounts of insulin to bring it down.
Over time, this constant demand for insulin leads to insulin resistance.
Then there is stress. I had no idea how much my stress levels were affecting my insulin glucose metabolism.
Stress triggers the release of cortisol, a hormone that raises blood sugar. Constant stress, combined with poor dietary choices, contributed to my insulin resistance, further damaging my glucose metabolism.
A lack of regular exercise didn’t help either.
Exercise plays a key role in helping your body use glucose more efficiently, but my sedentary lifestyle meant that I was missing out on one of the best natural ways to boost glucose metabolism and insulin sensitivity.
Scientific Explanation of the Metabolic Pathways Involved in Diabetes
Let us dive into the science of metabolic pathways involved in diabetes. In type 2 diabetes, the breakdown occurs primarily in two pathways: the insulin signaling pathway and the glucose transport pathway.
The insulin signaling pathway is responsible for “telling” your cells to take in glucose. When you eat a meal, insulin binds to receptors on the surface of your cells, activating a cascade of reactions that result in glucose transporters moving to the cell membrane.
These transporters act like gates, allowing glucose to pass from the bloodstream into the cell.
In people with insulin resistance, this pathway is disrupted.
The receptors on the cells become less responsive to insulin, which means fewer glucose transporters are activated. The result? Glucose stays in the bloodstream, and your metabolic glucose levels remain elevated.
The second disrupted pathway is the glucose transport pathway itself. In a healthy individual, glucose transporters efficiently move glucose from the blood into the cells.
However, in people with type 2 diabetes, the number and function of these transporters are impaired.
This further exacerbates the problem, as glucose continues to accumulate in the bloodstream, while the cells are starved for energy.
Additionally, scientific studies have shown that excess fat, especially around the abdomen, releases inflammatory markers that interfere with insulin’s ability to do its job.
This inflammation disrupts both the insulin signaling pathway and glucose transport, worsening insulin resistance and glucose metabolism in type 2 diabetes.
FAQs on Type 2 Diabetes & Glucose Metabolism
Q-1: How does type 2 diabetes disrupt normal glucose metabolism in the body?
A-1: Type 2 diabetes interferes with how the body processes glucose by causing insulin resistance. Normally, insulin signals cells in the muscles and fat to absorb glucose for energy. When cells become resistant, glucose remains in the bloodstream, leading to elevated blood sugar levels.
As per bestdietarysupplementfordiabetics.com, “The pancreas tries to compensate by producing more insulin, but over time this can strain or damage insulin-producing cells. Understanding how type 2 diabetes affects glucose uptake and insulin signaling helps explain why blood sugar control becomes challenging”.
Q-2: Why do my blood sugar levels spike even after eating healthy foods?
A-2: In type 2 diabetes, insulin release is often delayed and less effective, meaning glucose from food stays in the blood longer. Even low-glycemic or high-protein meals can cause noticeable post-meal spikes.
This is because insulin resistance in type 2 diabetes causes delayed glucose absorption in the muscles and fat cells. Monitoring blood sugar after meals helps identify which foods trigger spikes and allows for adjustments to improve glucose control.
Q-3: How does disrupted glucose metabolism affect my daily energy and fatigue?
A-3: When glucose cannot enter cells efficiently, energy production is reduced, leaving muscles and the brain under-fueled. Many people experience sudden fatigue, brain fog, or energy crashes, especially after meals.
These symptoms illustrate the impact of type 2 diabetes on energy levels and glucose utilization, emphasizing the importance of maintaining stable blood sugar for both physical and mental performance.
Q-4: Does type 2 diabetes alter liver function in glucose regulation?
A-4: Yes. The liver plays a crucial role in maintaining blood sugar between meals by storing and releasing glucose as needed. In type 2 diabetes, insulin resistance causes the liver to release glucose even when blood sugar is high.
This contributes to elevated fasting glucose and makes it harder to manage blood sugar throughout the day. Understanding how type 2 diabetes affects liver glucose production is essential for improving overall glucose control.
Q-5: Can improving insulin sensitivity restore normal glucose metabolism?
A-5: Absolutely. Lifestyle strategies such as regular exercise, balanced nutrition, weight management, and stress reduction enhance insulin sensitivity.
As cells respond better to insulin, glucose is absorbed more efficiently, fasting glucose levels stabilize, and post-meal spikes are reduced. Knowing how to improve insulin sensitivity naturally in type 2 diabetes can significantly support blood sugar regulation and reduce the risk of long-term complications.
Rebalancing Glucose Metabolism and Managing Type 2 Diabetes
Living with type 2 diabetes has taught me one crucial lesson: understanding how my body processes glucose is the key to managing the disease.
Type 2 diabetes disrupted my glucose metabolism by breaking the delicate balance between insulin and glucose. Over time, insulin resistance set in, leading to elevated blood sugar levels and the gradual breakdown of my body’s ability to use glucose efficiently.
But here is the good news: it is possible to rebalance your glucose metabolism with the right approach. The first step is to make lifestyle changes that directly address the factors contributing to insulin resistance.
This includes adopting a diet rich in whole grains, lean proteins, healthy fats, and plenty of fiber to stabilize blood sugar levels. Reducing sugar and processed foods is essential to prevent the spikes in blood sugar that cause overproduction of insulin.
Exercise, too, plays a critical role in improving insulin sensitivity. Even moderate activity, like walking or swimming, helps your muscles use glucose more effectively, lowering your blood sugar levels naturally.
Finally, managing stress through diabetes support groups, meditation, or yoga can help keep cortisol levels in check, reducing the negative impact of stress on glucose metabolism and insulin function.
I also recommend using best supplements to lower blood sugar.
In summary, while type 2 diabetes may have disrupted my glucose metabolism, the journey to recovery lies in understanding how these processes work and making changes that support balanced glucose levels.
By addressing diet, exercise, and stress management, I’ve been able to manage my condition and regain control over my glucose metabolism.
References: