Pancreas Transplant: The Controversial Cure for Diabetes No One Talks About
- admin
- September 2, 2024
- 3:33 pm
- No Comments

Diabetes is a condition that millions of people worldwide grapple with daily.
From managing blood sugar levels to dealing with the potential long-term complications, living with diabetes is no easy feat.
Yet, amidst the myriad of treatments available—like insulin therapy, lifestyle changes, and medications—there is one solution that remains largely under-discussed: the pancreas transplant.
While it may sound like a miraculous fix, this procedure is steeped in controversy, and its role in diabetes management is not as widely acknowledged as you might expect.
So, what’s the deal with pancreas transplants? Why aren’t more people talking about it? Let’s find out!
What is a Pancreas Transplant?
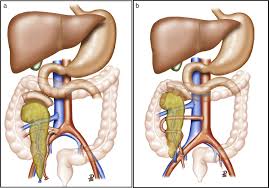
A pancreas transplant is a surgical procedure where a healthy pancreas from a donor is transplanted into someone whose pancreas no longer functions properly.
The pancreas plays a critical role in managing blood sugar levels by producing insulin, the hormone that regulates glucose in the bloodstream.
For individuals with type 1 diabetes, whose bodies can’t produce insulin, a pancreas transplant can, theoretically, restore normal insulin production and eliminate the need for insulin injections.
The Promise of a Cure
For many people with type 1 diabetes, a pancreas transplant offers something no other treatment can: the potential for a cure.
Unlike insulin therapy, which only manages the symptoms of diabetes, a pancreas transplant addresses the root cause—an underperforming or non-functioning pancreas.
According to bestdietarysupplementfordiabetics.com research, successful pancreas transplants can lead to long-term insulin independence and normalized blood sugar levels, drastically improving quality of life.
Moreover, a pancreas transplant can also help mitigate or even reverse some of the complications associated with diabetes, such as neuropathy or kidney damage.
The idea of not only managing but potentially curing diabetes is a powerful one.
However, this potential cure is not without its risks and complications.
The Risks Involved
While the promise of a cure is enticing, the reality of a pancreas transplant is much more complex.
First and foremost, the procedure itself is highly invasive. It requires major surgery, which comes with inherent risks such as infection, bleeding, and complications related to anesthesia.
But perhaps the most significant concern is the risk of organ rejection. Since the new pancreas comes from a donor, the recipient’s immune system may recognize it as a foreign invader and attempt to attack it.
To prevent this, patients must take immunosuppressive drugs for the rest of their lives.
These drugs help prevent rejection but also come with their own set of risks, including increased susceptibility to infections, higher chances of developing certain cancers, and other side effects such as cholesterol induced high blood pressure and kidney damage.
The long-term use of these medications can sometimes feel like trading one set of problems for another.
Limited Availability and Eligibility
Another factor contributing to the under-discussion of pancreas transplants is the limited availability of donor organs.
The demand for donor organs far exceeds the supply, making it challenging for many individuals to receive a transplant.
According to the United Network for Organ Sharing (UNOS), the waiting list for a pancreas transplant can be long, with many patients waiting months or even years for a suitable donor organ.
Moreover, not everyone with diabetes is eligible for a pancreas transplant.
The procedure is most commonly recommended for individuals with type 1 diabetes who also have severe kidney damage, a condition known as diabetic nephropathy.
In these cases, a pancreas transplant is often performed in conjunction with a kidney transplant.
Patients without kidney disease or with type 2 diabetes, where insulin resistance is a primary issue rather than insulin production, are typically not considered ideal candidates for a pancreas transplant.
Success Rates and Outcomes:
Despite the risks and challenges, pancreas transplants have a relatively high success rate.
According to a study published in the American Journal of Transplantation, one-year survival rates for patients and grafts (the transplanted pancreas) are over 90%, and many patients remain insulin-independent for years after the procedure.
The long-term outcomes are also promising, with many patients experiencing a significant improvement in their quality of life and a reduction in diabetes-related complications.
However, the success of a pancreas transplant depends on several factors, including the patient’s overall health, the quality of the donor organ, and the effectiveness of the immunosuppressive therapy.
Regular follow-ups and medical monitoring are essential to ensure the transplant continues to function well and to catch any potential issues early on.
The Ethical Debate
Pancreas transplants also raise ethical questions, particularly concerning the allocation of donor organs.
Given the scarcity of donor organs and the risks associated with immunosuppressive therapy, some medical professionals argue that pancreas transplants should be reserved only for those with the most severe cases of diabetes.
Others, however, believe that the potential for a cure justifies offering the procedure to a broader range of patients.
There is also the question of cost. Pancreas transplants are expensive, and not all insurance plans cover the procedure or the lifelong immunosuppressive therapy that follows.
This raises concerns about access and equity—should only those who can afford the procedure have the opportunity to potentially cure their diabetes?
Why Isn’t Everyone Talking About It?
Given the potential benefits of a pancreas transplant, you might wonder why it is not a more popular or widely discussed option for diabetes management.
The answer lies in the complexity of the procedure, the associated risks, and the stringent eligibility criteria. Pancreas transplants are not a one-size-fits-all solution.
They are typically reserved for the most severe cases of diabetes, where the potential benefits outweigh the risks.
For many individuals with diabetes, the daily management of the condition with insulin or liquid metformin medications remains a safer and more practical option.
Moreover, the success of other treatment options, such as insulin pumps and continuous glucose monitoring systems, has provided effective ways to manage diabetes without the need for invasive surgery.
These advancements in diabetes care have made the option of a pancreas transplant less necessary for many people.
FAQs on Pancreas Transplant for Controlling Blood Sugar
Q-1: Why is pancreas transplant considered a controversial option for diabetes treatment despite its potential to restore insulin production?
A-1: Pancreas transplant is controversial because, while it can restore natural insulin production and potentially cure diabetes, it involves significant risks such as rejection, infection, and lifelong immunosuppressant use. These risks, combined with the complexity of the surgery and limited donor availability, make it a less common and often debated treatment choice.
Q-2: How does pancreas transplant compare with islet cell transplantation, and why is this distinction rarely discussed?
A-2: Unlike islet cell transplantation, which implants only insulin-producing cells, a full pancreas transplant replaces the entire organ. The distinction is important because pancreas transplants typically have higher success rates but more surgical risks. The lack of discussion often stems from the medical community’s focus on less invasive alternatives and the nuanced patient eligibility criteria for each procedure.
Q-3: What ethical considerations contribute to the limited conversation around pancreas transplants as a diabetes cure?
A-3: Ethical concerns include allocation of scarce donor organs, prioritizing patients based on severity and prognosis, and balancing risks versus benefits. Since pancreas transplants are often reserved for patients with severe diabetes complications, debate arises over whether this approach is equitable or diverts organs from other critical needs.
Q-4: Can pancreas transplant eliminate the need for diabetes management entirely, and what factors influence this outcome?
A-4: While pancreas transplant can eliminate the need for insulin injections by restoring insulin production, success depends on factors such as transplant rejection rates, patient adherence to immunosuppressive therapy, and overall health. Some patients may still require ongoing monitoring and medication adjustments, meaning it’s not always a definitive cure.
Q-5: Why is public awareness about pancreas transplant as a diabetes treatment so low, and how could increasing education impact patient decisions?
A-5: Public awareness is low due to limited media coverage, the procedure’s complexity, and its designation primarily for severe cases. Increasing education could help patients understand the full spectrum of treatment options, weigh risks and benefits better, and advocate for personalized care decisions, potentially leading to more informed and hopeful management of diabetes.
Conclusion: A Controversial Cure?
So, is a pancreas transplant the controversial cure for diabetes that no one talks about?
In some ways, yes.
It offers the promise of a cure—a life free from insulin injections and the constant monitoring of blood sugar levels.
But this promise comes with significant risks, ethical dilemmas, and practical limitations that make it a less-than-ideal solution for many individuals with diabetes.
For those who are eligible and choose to undergo the procedure, a pancreas transplant can be life-changing. However, it is not a decision to be made lightly.
The complexities and controversies surrounding pancreas transplants are why it remains a less discussed and less utilized option in the world of diabetes management.
I am a Type 2 Diabetic and I prefer to include Natural Supplements to Lower Blood Sugar along with my regular diet.
As with any medical treatment, it is crucial to weigh the benefits and risks and to have open, informed discussions with healthcare providers to determine the best course of action for each individual case.
References: